Scam alert: Ads or websites claiming to have Medsafe approval or with the Medsafe logo are fake. Medsafe doesn’t endorse any health products, services or brands. Go to Medsafe for official information.
Cervical polyps
Key points about cervical polyps
- Cervical polyps are common and occur in about 4% of women.
- Cervical polyps usually cause no symptoms and are sometimes found during a smear test.
- However, some women may experience symptoms such as bleeding after sex, bleeding in between periods, bleeding after menopause or abnormal vaginal discharge.
- In most cases, cervical polyps are benign (not cancerous).
- The main treatment for cervical polyps is to have them removed.

Cervical polyps are small non-cancerous growths that form on your cervix.
The exact cause of cervical polyps is not known. Possible causes include:
- congestion of blood vessels in your cervix
- infection or chronic (long-term) inflammation of your cervix
- abnormal response to an increase in oestrogen levels.
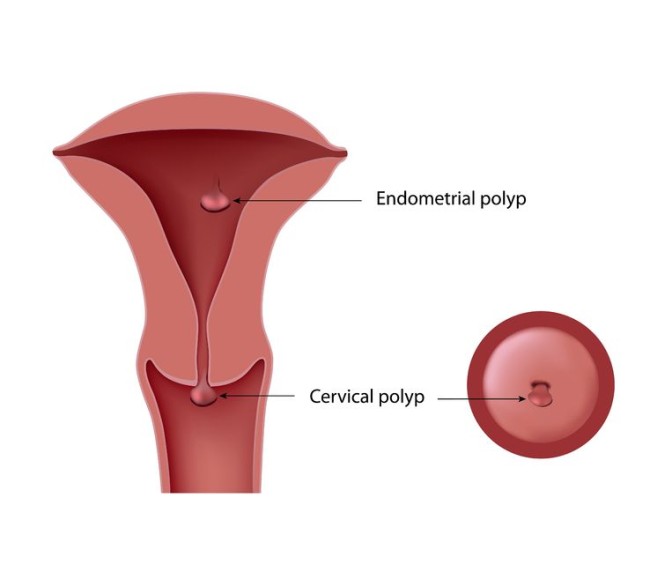
Image: A cervical polyp sitting just outside the cervical passage, which connects your vagina to your womb (uterus). Note: this image also shows an endometrial polyp within the womb. Source: 123rf.com
The common symptoms of cervical polyps include:
- unusual vaginal bleeding such as bleeding after sexual intercourse
- bleeding between your menstrual periods
- bleeding after menopause
- white or yellow mucous or discharge from your vagina.
Cervical polyps usually cause no symptoms and the polyps are only noticed during a routine cervical smear test.
Your doctor will ask you questions about your symptoms such as vaginal bleeding or discharge, your periods, your previous smear results and any gynae health issues in the past. Your doctor will then examine you, including inserting a speculum into your vagina to look for obvious polyps and taking a cervical smear.
Additional tests are not usually needed. However, if your doctor thinks that your polyps may have grown from your womb, or that removal of the polyps might be complicated, an ultrasound scan of your pelvis may be done.
It is recommended that cervical polyps be removed. This is usually a simple painless process and can be done in GP clinics.
If your polyp is small, it can often be removed by your doctor.
- To remove it, the polyp is gently twisted using an instrument called polyp forceps until the polyp tissue comes away from your cervix and is removed. Your polyp will then be sent to the lab for examination.
- After removal of your polyp, there may be light bleeding and slight cramping for a few days.
- You will need to have an examination and smear test 3 months after the polyp has been removed, even if your last smear test was normal.
- This is because the polyp blocks access to the cervical cells and the smear result may be a false negative, and to check that the polyp has been completely removed.
- Polyps can grow again so see your doctor if your symptoms return.
- If you still have abnormal vaginal bleeding after removal of a polyp, other tests may be done to find out the causes.
If a polyp is larger than 2 cm, has a large base or is otherwise difficult for your doctor to remove, you are likely to be referred to a gynaecology specialist for assessment and treatment.
- Removing the polyp will ease symptoms such as bleeding after intercourse or bleeding between your menstrual periods.
- If not removed, a polyp may continue to grow.
- In a small number of women (between 2 and 15 in every 1000), the polyp may become abnormal and develop into cancer.
The following links provide further information about cervical polyps. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Cervical polyps(external link)(external link) HealthInfo Canterbury, NZ
Common problems of the cervix(external link)(external link) Patient Info, UK
Apps
References
- Cervical polyps(external link)(external link) Auckland Regional HealthPathways, NZ
- Investigating and managing abnormal vaginal bleeding(external link)(external link) BPAC, NZ
- Cervical Polyps(external link)(external link) MSD Manual, Professional Version, US
- Uterine cervix and common cervical abnormalities(external link)(external link) Patient Info, UK
Clinical pathways and guidelines
Investigating and managing abnormal vaginal bleeding(external link) BPAC, NZ
Cervical polyps(external link) MSD Manual, Professional Version, US
Uterine cervix and common cervical abnormalities(external link) Patient Info, UK
Apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Arna Letica, FRNZCGP, Auckland
Last reviewed:
Page last updated:





