If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Cervical cancer | Mate pukupuku waha kōpū
Key points about cervical cancer
- Anyone with a cervix can get cervical cancer. Screening and immunisation offer the best protection against it.
- Cervical cancer can be cured if it’s found and treated early.
- Aotearoa New Zealand has a very effective programme for cervical screening and this has reduced the rate of cervical cancer by about 50% since screening started in 1990.
- See your healthcare provider if you have bleeding outside of your period for any reason, but especially after sex.

Cervical cancer (mate pukupuku waha kōpū) is cancer that forms in your cervix. The cervix is the lower part of your uterus (womb) – it’s sometimes known as the neck of the womb.
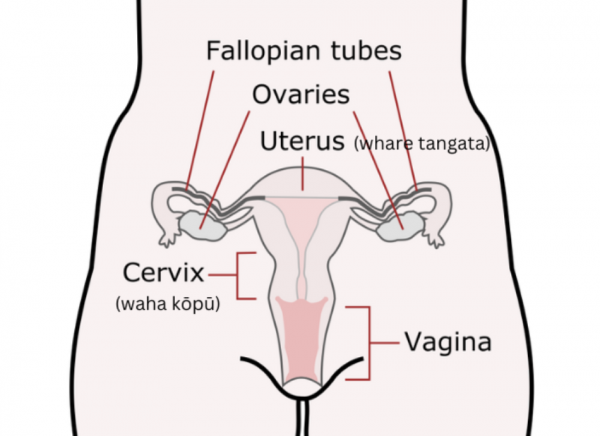
Image credit: Open Clipart
Cervical cancer is almost always caused by a virus called the human papillomavirus (HPV). There are several types of HPV that cause cervical cancer – called high risk HPV. There’s now a vaccine that can protect against certain types of HPV, including most of those that cause cervical cancer.
There are 2 main types of cervical cancer – squamous cell carcinoma (most cervical cancers are of this type) and adenocarcinoma. They’re named after the type of cell where the cancer started.
Cervical cancer is almost always caused by several types of a virus called human papillomavirus (HPV). The virus spreads through sexual contact and most people who are sexually active will be exposed to some type of it. Most HPV infections clear by themselves, but some high-risk types can cause cell changes on the cervix that may lead to cervical cancer 10 to 20 years after infection. Other types can cause genital warts, but these don't lead to cancer.
There are things that can increase your risk of cervical cancer. These include if you:
- smoke
- have had multiple sexual partners
- have used birth control pills for a long time
- have a weakened immune system.
Cervical cancer may not cause any symptoms at first, which is why you should take part in the National Cervical Screening Programme. Cervical screening can detect high risk HPV infection and early cell changes that can indicate that cancer may develop within your cervix (invasive cancer).
If early cell changes develop into invasive cervical cancer, the most common signs include:
- vaginal bleeding between your menstrual periods
- bleeding after sexual intercourse
- pain during sexual intercourse
- unusual vaginal discharge
- vaginal bleeding after menopause
- excessive tiredness
- leg pain or swelling
- low back pain.
All these symptoms are common to many conditions and may not mean you have cervical cancer. However, if you have these symptoms, have them checked by your healthcare provider.
See your healthcare provider if you have bleeding (that’s not due to your period) for any reason, but especially if you bleed after sex.
HPV testing
Most people with cervical cancer are identified through HPV testing during cervical screening. They don’t usually have any symptoms and are found to have very early cervical cancer – which is easier to treat and less likely to cause long-term problems.
If high risk HPV is detected in your vaginal swab at cervical screening, you'll need a follow-up check. Depending on the type of HPV detected, you might need a cervical sample test (a smear test) or you might need a referral to a specialist for a colposcopy.
Cervical sample test
If high risk HPV infection is found through your cervical screening test, or if you have symptoms that suggest you may have cervical cancer, your healthcare provider will examine you (this may include vaginal, pelvic and rectal exams) and take a cervical sample (used to be known as a smear test).
In a cervical sample test, some of the cells from the surface of the cervix are taken and examined under a microscope to look for abnormal cells. HPV testing will also be done if you haven’t had a screening test. Read more about these tests on the cervical screening page.
Colposcopy and biopsy
If abnormal cells are found in your cervical sample test, you may be referred to a specialist doctor (usually a gynaecologist or an oncologist). This doesn’t necessarily mean there is cancer present – for a cancer to be present the abnormal cells must start to grow into (invade) the cervix.
A specialist doctor will do a colposcopy which involves looking at your cervix using a magnifying device called a colposcope. If necessary, they’ll take a small piece of tissue (a cervical biopsy) from any areas that look abnormal. The tissue sample will be examined under a microscope to look for cancer.
LLETZ, cone biopsy
LLETZ (Large Loop Excision of the Transformation Zone) is a procedure that removes abnormal cells from your cervix. The small pieces of tissue that are removed are sent to the laboratory to test for cancer.
A cone biopsy is where a small cone-shaped part of your cervix that contains the abnormal cells is removed. The cells are sent to the lab for testing.
LLETZ and cone biopsy can also be used for the treatment of non-invasive or very early stage cervical cancer (see the treatment section below).
MRI, CT and PET scans
If the results of the tests above suggest that you may have cervical cancer and that there's a risk the cancer may have spread, further tests are done to find out how widespread the cancer is (what stage it is). This makes it possible to plan the best treatment. The most common tests are:
- MRI scan – this is the best way of seeing how far the main part of the cancer has spread through the cervix and how close it is to the bladder and the bowel.
- CT scan – this scan is very good for looking at lymph nodes in your pelvis and chest which is where the cancer is most likely to spread to first.
- PET scan – this is often combined with CT scanning to give more detailed information about your cancer.
All cancers are classified by how far they have progressed or the stage that the cancer has reached. The higher the stage, the further the cancer has spread. The staging for cervical cancer is as follows:
- Stage 1 – when there are cancer cells inside the cervix but they haven't spread further.
- Stage 2 – when the cancer has spread beyond the cervix into the surrounding tissue, but hasn't reached the tissues lining the pelvis (pelvic wall) or the lower part of the vagina.
- Stage 3 – when the cancer has spread into the lower section of the vagina and/or into the pelvic wall. It may also have spread to nearby lymph nodes.
- Stage 4 – when the cancer has spread into the bowel, bladder or other organs, such as the lungs or distant lymph nodes.
There are different treatment options for cervical cancer depending on things such as how far the cancer has spread, your age and what other health conditions you have. Treatment may also take into consideration whether you wish to have children in the future.
Treatment for abnormal cells
If the results of cervical screening show that you have abnormal cells that are of concern, there are different options available to remove the cells from your cervix. Treating abnormal cells makes it unlikely that you’ll develop invasive cervical cancer in the future. The treatments include:
- LLETZ, laser therapy or diathermy – these procedures are done under local anaesthesia and use an electrical wire, laser beam or heat to remove or destroy the abnormal cells. With LLETZ, the tissue removed is sent to the laboratory for testing.
- Cone biopsy – this is where a small cone-shaped part of your cervix that contains the abnormal cells is removed. It can be done under local or general anaesthesia. The tissue removed is sent to the lab for testing.
- Total hysterectomy – this is an operation to remove your uterus and cervix and isn’t commonly done for the treatment of abnormal cervical cells.
After treatment, you’ll be seen for follow-up, which includes HPV and cervical sample testing, and your healthcare provider will let you know when you can re-start regular cervical screening if appropriate.
Treatment of invasive cancer
If you have invasive cervical cancer (stages 1 to 4), treatments include the following:
- LLETZ or cone biopsy – these might be done to remove the abnormal cells in your cervix if you have very early cervical cancer and if you wish to have children in the future.
- Trachelectomy – this is an operation to remove your cervix. If you have early cervical cancer and want to have children, if might be possible to leave enough of the cervix behind so that you might be able to get pregnant and carry a child.
- Hysterectomy – this is an operation to remove your cervix and uterus and often your fallopian tubes and ovaries as well. In early stage cervical cancer, hysterectomy is the main form of treatment. If the cancer is very early, this is all that’s needed. The lymph nodes near your cervix will be checked carefully and if these lymph nodes have cancer cells in them, you’ll also be treated with radiation therapy. A radical hysterectomy is an operation where the tissue around the cervix and the lymph nodes in the pelvis are also removed.
- Radiotherapy – radiation treatment is very useful if you have cervical cancer. There are different types of radiation used:
- Brachytherapy delivers radiation directly inside or near the cancer. It can be used before surgery to decrease the size of the cancer and to increase the chances that surgery will remove all the cancer.
- External beam radiotherapy is used to treat a wider area, including cancer cells that have spread to the lymph system or formed metastases (tumours in other parts of the body).
- Chemotherapy – anti-cancer drugs are often used with radiotherapy and can be used before or after surgery.
- Immunotherapy – pembrolizumab (Keytruda) can be used in the treatment of some people with cervical cancer. It’s available in Aotearoa New Zealand but isn’t funded for the treatment of cervical cancer.
If you’ve been diagnosed with cervical cancer there are things you can do to help care for yourself:
- Listen to your body – learn to be kind to yourself, find a balance between rest and activities or exercise you can manage, and eat healthily.
- Talk to people who can support you with the challenging feelings you may experience. You could talk to family or friends, or a professional such as a therapist or psychologist.
- Stay connected with those closest to you – keep communication lines open and let your loved ones support you.
- Consider your spiritual wellbeing/wairuatanga – this might come from religious beliefs, your cultural upbringing, or your core values and principles. This can help you find a clearer sense of what’s important to you if you’re living with cancer.
- You may also want to discuss fertility or relationship issues (including the effects of treatment on fertility) – ask your care team to put you in touch with people who can help with these.
The likely outcome or course of cervical cancer depends on many factors including:
- the type of cervical cancer you have
- the stage of your cancer
- your age and general health, and
- whether your cancer is newly diagnosed or has come back after treatment.
Your oncologist (doctor who specialises in cancer) is the best person to talk to about your specific situation.
Most people who have early-stage cervical cancer will be cured, but the cancer can come back. Usually this happens within 5 years of treatment. In most cases, you’ll be seen every year to check for any signs that the cancer has reappeared. Although it’s much more difficult to cure cervical cancer if it returns, it’s still possible to delay its growth and improve your quality of life. This is a difficult time for you and your whānau and all cancer units in Aotearoa New Zealand have special teams to help you through this.
The best way to avoid getting cervical cancer is by being vaccinated against HPV infection and having regular cervical screening.
- If you’re 9 to 26 years of age, you can be immunised with the free HPV vaccine to protect you from cancer-causing HPV infection. This decreases your risk of cervical cancer by 90%. If you don’t fit into the 9 to 26 age range you can still be immunised but you’ll have to pay for the vaccination. The vaccine doesn’t protect against all HPV types, so even if you’ve been immunised with the vaccine you must still continue to have cervical screening if you’re eligible for this.
- Have regular cervical screening as part of the National Cervical Screening Programme. This is now done by an HPV primary screening test using a vaginal swab which is tested for the presence of HPV. If HPV is found, further testing can look for abnormal cervical cells which can be treated before they turn into cancer (see above).
- Also, don’t smoke, or quit smoking if you do smoke, to help reduce your chance of getting cervical cancer.
If you have cancer, including cervical cancer, there are organisations that can support you and your whānau.
The New Zealand Cancer Society(external link) provides practical and emotional support and information to people with any kind of cancer at any stage of their cancer experience. Visit the Cancer Society website(external link) or phone 0800 226 237 for advice and information. They have many resources(external link) including information about coping with side effects of treatment, dealing with emotions, and living with cancer.
At Healthpoint(external link) you can find Aotearoa based services that provide support for you and your whānau if you’ve been affected by cancer.
Look Good Feel Better(external link) provides free wellbeing services to any person with any cancer at any stage.
Rangitāne o Tamaki nui a Rua(external link) provides a wide range of support services to whānau in the Tararua region. Services include He Mate Pukupuku Cancer Care Coordination which supports and advocates for whānau with their cancer journey. They work with the Cancer Society, local and secondary care providers, clinical services, and palliative care. Phone 06 374 6860 or email [email protected].
Cervical cancer(external link) Cancer Society NZ
HPV and Cervical Cancer(external link) National Screening Unit NZ
Cervical cancer(external link) Talk Peach Gynaecological Awareness, NZ
Brochures
Understanding cervical cancer(external link) Cancer Council Australia, 2023
Cervical screening – understanding test results(external link) National Cervical Screening Programme, NZ, 2023 Also available in te reo Māori(external link)
Colposcopy – what you need to know(external link) National Cervical Screening Programme, NZ, 2023 Also available in te reo Māori(external link)
Apps
References
- Cervical cancer(external link) Cancer Society, NZ, 2024
- Cervical cancer – early detection and referral(external link) BPAC, NZ, 2024
- Cervical cancer(external link) Te Aho o te Kahu | Cancer Control Agency, NZ
- Treatment options for cervical cancer(external link) Cancer Research UK
- Cervical cancer prognosis and survival rates(external link) National Cancer Institute, US, 2023
- Cervical cancer – stages(external link) University of Rochester Medical Center, US
- Cervical screening – treatment for abnormal cells(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
- Chemotherapy + radiotherapy – cervical cancer treatment information(external link) Gynaecology Oncology Unit Christchurch Hospital, NZ, 2021
- Tests for cervical cancer(external link) Cancer Research UK
Guidelines for cervical screening in NZ(external link) Health New Zealand | Te Whatu Ora, 2023
Cervical cancer – early detection and referral(external link) BPAC, NZ, 2022
Gynaecological cancers – follow-up and surveillance(external link) BPAC, NZ, 2023
Gynaecological cancers – follow-up and surveillance(external link) B-QuiCK BPAC, NZ
Cervical cancer(external link) B-QuiCK BPAC, NZ
Brochures

Time to Screen, NZ, 2023

Time to Screen, NZ, 2023
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Jessica Dunning, Obstetrician and Gynaecologist, Te Toka Tumai Auckland and Auckland Gynaecology Group.
Last reviewed:





