There are many treatments for vulvodynia, but what works for someone else may not help you. Work with your doctor to find what is best for you. Even though there is no cure, treatment can help you feel better and lead a full and active life. Vulvodynia goes away on its own in about 40% of women.
Self-care
Here are a few things you can try to help relieve immediate pain and soreness:
- To relieve itching and pain, apply a cold water compress or cool gel packs to the vulva. Don't scratch the area.
- For pain when sitting, using a doughnut-shaped cushion can help.
- Vaginal lubricants may soothe the area and help moisturise the vulva. Talk to your pharmacist about a suitable product.
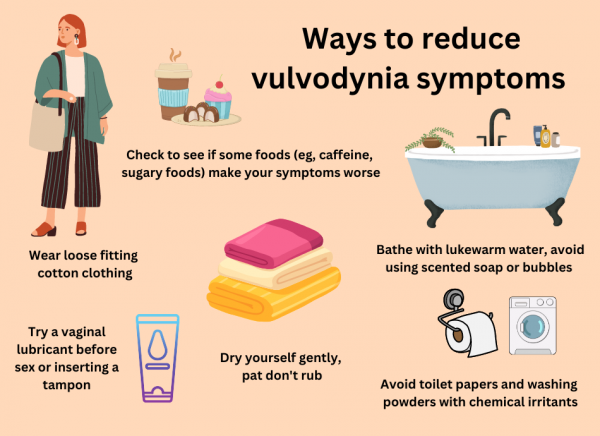
Here are a few lifestyle tips may help reduce symptoms of vulvodynia:
- Bathing
- Avoid scented soaps, shower gels, bubble bath, vaginal sprays or douches, as these can irritate your skin. Instead of scented soap or shower gel, rinse with water only or use an emollient as a soap substitute. Read more about wash-off emollients as soap substitutes.
- Avoid hot baths or showers – use lukewarm water instead.
- Gently pat the area dry. Don't rub harshly with a towel.
- Some toilet papers and washing powders may have chemicals in them that can also irritate the skin.
- Wear loose-fitting cotton clothes. Avoid nylon and other fabrics that hold moisture close to the skin. This may cause irritation and allow an infection to start.
- Try using a vaginal lubricant such as Sylk® before intercourse or before inserting a tampon. When choosing a vaginal lubricant, avoid those with alcohol or preservatives. Avoid using KY Jelly.
- Stay active, but limit exercises that can irritate the vulva, such as bike riding or horseback riding. Use petroleum jelly before swimming to provide protection from chlorine.
- For some women, certain foods make symptoms worse (eg, caffeine, foods high in sugar, acidic foods and processed foods). If you suspect that some foods may be triggering your symptoms, cut out one food at a time and make a note of your symptoms.
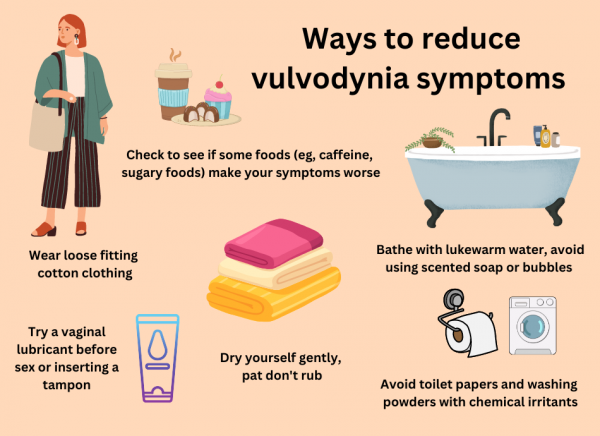
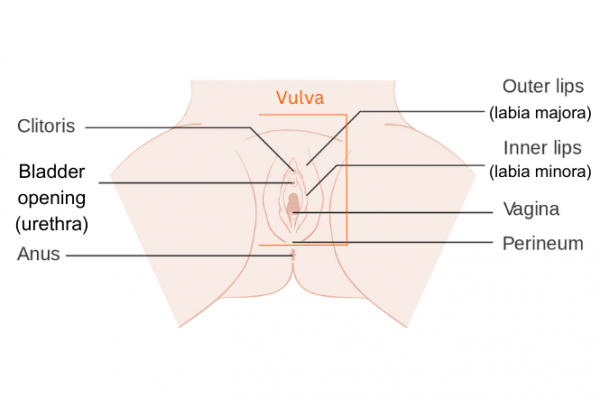
Image credit: Healthify He Puna Waiora, NZ
Physiotherapy
Pelvic floor exercises (such as squeezing and releasing your pelvic floor muscles) to help relax the muscles around your vagina may be helpful. In addition, specialised physiotherapists can help with pain symptoms through specific exercises, stretches and other techniques.
Medications
Some women have found the following medicines to be helpful in relieving the symptoms of vulvodynia:
Local anaesthetic cream
Applying a local anaesthetic cream such as lignocaine 2% to your vulva about 10 minutes before sex may make it more comfortable. To stop the gel getting on your partner, either wipe it off just before having sex or ask your partner to wear a condom (if using condoms, use latex-free ones as latex condoms can be damaged by lignocaine). If your pain is more constant, applying lignocaine regularly throughout the day may help. It can also be used overnight. A tip is to put some on a cotton make-up removal pad and put it onto the sore area so it's held in place by your underwear.
It's very common to have some burning when the lignocaine is initially applied which can last several minutes before going numb. Try to give the lignocaine time ito work, but if the burning continues for 10 minutes, wash it off thoroughly.
Hormone creams
Hormone creams like oestrogen vaginal cream, applied to the vulva, may be helpful in relieving vaginal dryness in some women.
Medicines that block nerve impulses
Several medications that block nerve impulses can help to relieve the pain, such as:
- antidepressants called amitriptyline and nortriptyline:
- possible side effects include drowsiness, weight gain and dry mouth.
- anti-seizure medicine called gabapentin:
- possible side effects include dizziness, drowsiness and weight gain.
Your healthcare provider will probably start you on a low dose and gradually increase it until your pain subsides. You may need to take the medication for several months.
Psychological support
It may be helpful to see a counsellor or a sex therapist to support you through this journey. Your healthcare provider should be able to help you find local providers. There is more information regarding this on the Vulvodynia Support NZ website.(external link)
Apps reviewed by Healthify
You may find it useful to look at some Women's health apps.