If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Vaginismus
Key points about vaginismus
- Vaginismus is the spontaneous tightening of muscles around your vagina, making it difficult or impossible to use tampons or have intercourse.
- Because it’s spontaneous you can't control it.
- It affects about 7% of people with a vagina and is more common in younger women, but can happen at any age.
- There can be a physical reason for vaginismus, such as repeated urinary tract infections or post-menopausal changes. It can also be psychological due to misinformation, trauma or a past negative experience.
- Treatment can be very successful so don’t put up with it, ask your healthcare provider for help.

Vaginismus is when the pelvic floor muscles around your vagina tighten without you choosing to tighten them. It’s called involuntary or automatic tightening.
There are 2 different types:
- Primary vaginismus – when you have never been able to put anything inside your vagina.
- Secondary vaginismus – when you were able to use tampons or have sex in the past, but can’t anymore. This may be a result of surgery, trauma or some sort of treatment such as radiation therapy.
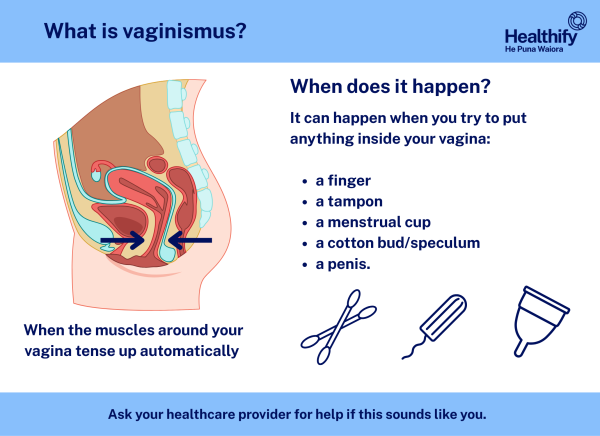
Image credit: Healthify He Puna Waiora
It can be painful and can make it hard or impossible to insert a tampon or have vaginal sex. Vaginismus can make it painful to have vaginal intercourse – this is known as dyspareunia.
Vaginismus can happen for various reasons, some are physical, others are psychological.
It’s more common in younger women (teens to early 30s) but anyone with a vagina can get it. It can also happen after menopause. It affects about 7% of women.
What vaginismus is not
- It’s not the pain you might feel the first few times you use a tampon – especially if you get the angle wrong! If you need help, find out more about how to use tampons.
- It’s not the pain or discomfort you feel when you are beginning to have vaginal intercourse. This might be because it’s a new experience for your body or because you haven’t been prepared (and don’t have enough vaginal lubrication) by foreplay before trying to have sex.
But if you continue to have pain and a feeling that your vagina is closing up, making it impossible for you to insert a tampon or finger, talk to a healthcare provider. If you don’t get help the problem may get worse and be harder to treat as time goes by.
The main symptom is discomfort, pain, or a feeling of 'blockage' due to the tightening of the muscles around your vagina making your vagina contract, narrowing the entrance. It can cause pain (burning or stinging) when you try to put anything into your vagina. You may also feel anxious or scared because you’ve experienced pain in a similar situation before. This can make it worse, and make you unable to use tampons or reluctant to have sex.
When can it happen?
It can happen when you try to put something inside your vagina, such as a tampon, a sex toy, a menstrual cup, or a finger. Or it can happen when you’re:
- having an internal examination
- having a cervical screening test
- having sex
- just thinking about these things happening.
Vaginismus may happen due to physical and psychological reasons.
Physical reasons
Most women with vaginismus don’t have a physical abnormality, but there can be physical reasons. These can include:
- health conditions such as thrush or recurrent urinary tract infections
- sexually transmitted infections (STIs)
- changes after menopause such as genitourinary syndrome of menopause which makes your vagina less elastic and lubricated.
Psychological reasons
These can include:
- past trauma from having a baby
- feeling negative about sex
- sex having been traumatic or painful in the past
- sexual assault, abuse or family violence
- a previous painful vaginal examination
- fear of getting pregnant
- relationship problems
- anxiety or depression.
Lack of arousal can also be a cause if your body isn’t prepared for intercourse.
Video: What is vaginismus? A psychosomatic reaction (6:26 mins)
Your healthcare provider will ask you about your symptoms, when they started, when they are likely to happen and what the triggers are. You'll also be asked about your sexual history, if you have one, and whether you’ve experienced any abuse or sexual trauma.
They're also likely to examine you with a pelvic exam, as they'll be able to see a muscle contraction. You may find this difficult, but they'll be careful and sensitive to your problem. Read more about pelvic exams and how to make them easier.
There are a few different ways of treating vaginismus.
- Education – it helps if you have a good understanding of your anatomy and what’s happening when you have vaginismus.
- Counselling – talking to somebody about when it happens and how it’s affecting your life can help. Involving your partner will help them understand and learn how to support you as well. A counsellor who works with sexual disorders may be helpful.
- Relaxation techniques – learning how to relax may help you to manage your vaginismus and feel more able to be touched and have intercourse.
- Vaginal dilators – these are cone-shaped objects that come in different sizes. With training, you place them inside your vagina – starting with a small one and moving up in size. The dilator gradually helps your vaginal and pelvic floor muscles to relax, allowing you to build up to using tampons and having intercourse.
- Pelvic floor exercises – it may help to see a physiotherapist who specialises in pelvic floor techniques. They can help you learn stretching and relaxation exercises and help you gain control of your pelvic floor muscles.
Be kind to yourself and understand that it’s not that there’s something wrong with you, you can’t help it and you’re not alone. It’s important that you talk to your healthcare provider as soon as you can. They can refer you to other healthcare providers, such as a counsellor, sex therapist or physiotherapist as needed.
- Get to know your own body.
- Learn what helps you to relax, eg, meditation, relaxation techniques, breathing exercises – especially belly (diaphragmatic) breathing.
- Touch yourself if you can, starting with the outside of your pubic mound and gradually moving towards putting a clean finger into your vagina.
- If you have a partner, try to be open with them about what’s happening. If you can’t have intercourse but are able to let them touch you, you can both enjoy an intimate relationship that doesn’t include penetration.
- Do any exercises your healthcare providers recommend.
- Use your healthcare provider and your partner for support.
With the right support and treatment there’s no reason why you can’t be cured of vaginismus and go on to have a normal sex life – many women do.
If there’s a medical reason why you have developed vaginismus it can be treated. If it’s to do with anxiety, lack of knowledge or trauma, counselling and exercises should help you. It may take a while.
Read about Amanda’s life with severe vaginismus(external link).
Video: I suffered with vaginismus for 10 years of marriage and it took over my life (3:53 mins)
Rashi talks about her experiences of vaginismus before she found a treatment centre that could help her.
Brochures
Vaginismus(external link) Jean Hailes for Women’s Health, Australia, 2023
Self-help guidance for vaginismus and pain with penetrative sex(external link) NHS, UK, 2023
References
- Vaginismus(external link) Health Direct, Australia, 2023
- Vaginismus(external link) NHS, UK, 2024
- Tight and painful vagina(external link) The Royal Women’s Hospital, Australia,
- Sexual pain (dyspareunia) – a patient’s guide(external link) Family Doctor, NZ
- How to treat vaginismus at home(external link) The Pelvic Hub, US
- What is vaginismus?(external link) Healthline, US, 2020
Brochures

Vaginismus
Jean Hailes, Australia, 2023
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trsut.
Reviewed by: Dr Alison Payne, Specialist General Practitioner, Martinborough
Last reviewed:






