The image below shows the anatomy of the testicle.
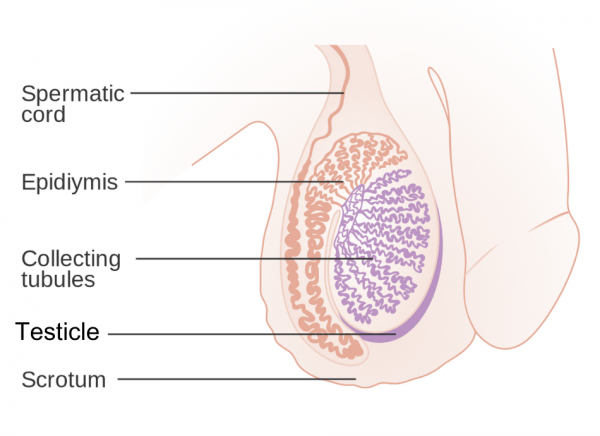
Image credit: CRUK via Wikimedia Commons
There are many reasons why your testicles may develop a lump or become swollen.
The most common causes include:
- enlarged veins within the scrotum or a build-up of fluid around the testicle (called a hydrocoele, pronounced hi-dro-seel)
- cysts caused by a collection of fluid in the epididymis (a coiled tube that lies beside each testicle and stores and carries sperm)
- inflammation of the epididymis and testicles, often caused by infection – see epididymo-orchitis
- a hernia – where fatty tissue or a part of your bowel pokes through into your groin.
A less common but more serious cause could be testicular cancer. You should always see a healthcare provider if you notice any lumps or swelling in your testicles. If it's painful, seek advice urgently.
See your healthcare provider immediately if you have sudden, unbearable pain in your testicles or abdomen (tummy). This could be a sign that your testicle has become twisted, which needs urgent hospital treatment.
Otherwise, see your healthcare provider if you have:
- a lump in your testicles – this can be a sign of testicular cancer and it's easier to treat if it’s found early
- red or swollen testicles
- a change in the shape or feel of your testicles
- an ongoing ache, pain or discomfort in your testicles.






