If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Plantar fasciitis
Key points about plantar fasciitis
- Plantar fasciitis is a common cause of heel or foot pain.
- It's often caused by repeated strain on the thick band of tissue that connects your heel to your toes along the bottom of your foot.
- You’re more likely to damage this tissue if you’re middle-aged, overweight, pregnant, physically active, have a job that requires you to stand for long periods, or if you wear flat shoes, such as jandals.
- There are things you can do to help relieve the pain and heal your foot.
- You can also reduce your risk of plantar fasciitis by maintaining a healthy weight and wearing appropriate footwear.

Plantar fasciitis is a condition that affects the thick band of tissue (called the plantar fascia) that connects your heel to your toes along the bottom of your foot. It's a common cause of heel or foot pain and is often seen in people who do a lot of running, jumping or dancing, but it can affect anyone.
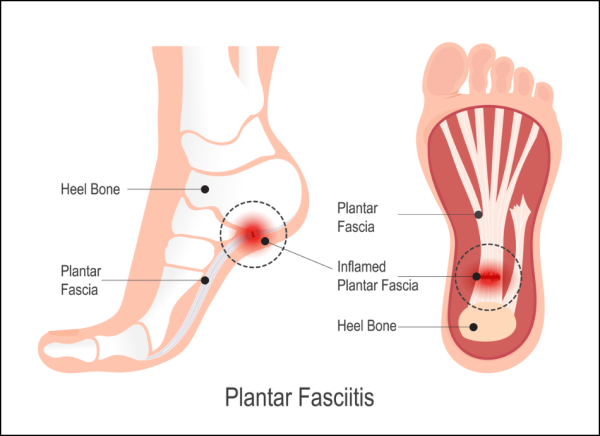
Image credit: Depositphotos
There are things you can do to help relieve the pain and heal your foot. You can also reduce your risk of plantar fasciitis by sticking to a healthy weight and wearing appropriate footwear.
Plantar fasciitis is caused by repeated small injuries that cause tiny tears in the plantar fascia tissue that runs under your foot. This tissue supports the arch of your foot and acts as a shock absorber in your foot.
It can also be caused when the plantar fascia tissue is suddenly injured or becomes inflamed. Anything that puts extra strain on your feet can cause plantar fasciitis.
You’re more likely to get plantar fasciitis if you:
- have flat feet or high-arched feet
- have an unusual way of walking, such as rolling your feet inwards
- are overweight
- are middle-aged
- wear badly-fitting or flat shoes or shoes that don't support your feet well
- stand, run, jump or dance on hard surfaces
- get an injury, such as a stress fracture
- have a medical condition such as diabetes or some types of arthritis
- are on your feet for long period s of time, eg, in retail or as a nurse
- walk, run or stand a lot when you're not used to it
- quickly increase the amount or intensity that you exercise
- have a tight Achilles tendon, or tight calf muscles.
There may be no obvious reason for developing plantar fasciitis, particularly if you're an older person.
The main symptom of plantar fasciitis is pain in your heel. The pain may be sharp or dull eg, stabbing or aching. You may also have an ache along the sole of your foot.
The pain is usually worse when you take your first steps in the morning, after you’ve been sitting or standing for a long time, or after exercising.
The pain improves with activity but worsens by the end of the day. It may be worse if you walk barefoot or when walking up stairs.
Your healthcare provider will ask you questions about your symptoms and will check for areas of tenderness in your foot. The location of the pain may help them make the diagnosis.
If they think your pain may be caused by another problem, such as a stress fracture or a pinched nerve, your healthcare provider might suggest an X-ray or ultrasound. Sometimes, particularly if the pain isn't settling with self-care, you may need to see a specialist. They may request magnetic resonance imaging (MRI).
If your pain is affecting both feet, unusual or prolonged your healthcare provider may also suggest you have blood tests to look for other causes.
Most people with plantar fasciitis recover with self-care treatments.
- Rest your foot as much as possible. Avoid running, too much walking and standing for long periods, particularly on hard surfaces. You could try other types of exercise such as cycling, swimming or aqua jogging.
- Use an ice pack under your foot for 20 minutes at a time especially if you get pain after being on your feet a lot.
- Ice and massage your foot at the same time – to do this, fill a 600ml plastic bottle with water, put it in the freezer and when it’s solid, roll the bottle under your foot (see the video below).
- Massage your foot by rolling a golf ball underneath it (see the video below).
- Lose weight if you’re overweight.
- Wear shoes with good cushioning and arch support, or use heel pads or arch supports (eg, from your pharmacy or podiatrist) in your shoes.
- Use night splints or tape on your foot at night. You can get these online or at some pharmacies.
- Stretch your Achilles tendon, calf muscles and plantar fascia (the underside of your foot) every day (see videos below).
- Strengthen your calf and foot muscles (see videos below).
- Take pain relievers such as paracetamol or ibuprofen to help ease pain and inflammation. Topical anti-inflammatories such as Voltaren gel may also help.
Video: Instant foot pain relief – 5 exercises to fix your plantar fasciitis
(Tone and Tighten, US, 2024)
Video: Foot pain – inflammation control
(Patient, UK, 2018)
Video: Foot pain – stretches
(Patient, UK, 2018)
Most people with plantar fasciitis recover within a year with self-care treatments including rest, massage, stretches and strengthening, good footwear and pain relief (see above).
Your healthcare provider may refer you to a podiatrist or physiotherapist. They can teach you stretching exercises for your calf muscles and plantar fascia, or give you ideas for how to change the way you exercise and do other regular activities. They may make suggestions about your footwear or provide insoles to put in your shoes. You can also refer yourself to a podiatrist and physiotherapist.
Find a podiatrist(external link) or a physiotherapist(external link).
However, if these simple measures don’t work after 3 to 6 months, you may be given a steroid injection. Steroid injections can relieve the pain temporarily but do have some risks – these need to be discussed with your healthcare provider.
Other options, if other treatments haven't been successful, is low level laser therapy (LLLT) or extracorporeal shock wave therapy. Shockwave therapy uses a machine to pass high energy sound waves through your skin to treat the affected area. In rare cases surgery may be considered, for example if your pain hasn’t improved after 12 months.
- Maintain a healthy weight, lose weight if you're overweight.
- Wear appropriate footwear, especially shoes that support and cushion your arches and heels and that have a low-to-moderate heel.
- Try orthotics (special inserts you can wear inside your shoes) if you have problems such as flat feet or high arches. You can buy orthotics at your pharmacy, or talk to a physiotherapist or podiatrist for specific advice.
- Warm up and cool down after exercise.
- Regularly stretch your calf and your plantar fascia (the underside of your foot) and Achilles tendon, especially before you exercise.
- Strengthen your feet and lower leg muscles, eg, with toe curls and calf raises.
- Avoid running or walking on hard surfaces.
- Change your walking and running shoes regularly.
- If you feel pain in your foot, follow the first aid RICE procedure of rest, ice, compression and elevation.
- Avoid over-training. If you want o increase the distance you walk or run, do it gradually over weeks to months.
Apps reviewed by Healthify
You may fid it useful to look at some nutrition, exercise and weight management apps.
Plantar fasciitis generally settles within 12 months if you keep up with the self-care treatments, including stretching exercises, mentioned above. You should try and do as many of these things in combination to help speed up your recovery time.
It’s best to make a gradual return to any sport and be guided by your symptoms. You can keep up your fitness by doing non-weight-bearing activities such as cycling or swimming.
Plantar fasciitis and heel pain(external link) Podiatry NZ
Heel pain(external link) NHS Choices, UK
Brochures
Plantar fasciitis advice and management – information for patients(external link) NHS, UK, 2022
References
- Plantar fasciitis(external link) Auckland Health Pathways, NZ, 2019
- Plantar fasciitis – heel and foot pain(external link) Patient Info, UK, 2024
- What causes plantar fasciitis?(external link) Patient Info, UK, 2023
- Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis – a randomized trial(external link) Arch Intern Med. 2006;166(12):1305–1310
- Uden H, Boesch E, Kumar S. Plantar fasciitis – to jab or to support? A systematic review of the current best evidence(external link) J Multidiscip Healthc. 2011;4:155–164
- Shockwave therapy(external link) NHS, UK, 2019
- David JA, Sankarapandian V, Christopher PRH, et al. Steroid injections for painful soles of heels in adults(external link) Cochrane Review, 2017
- Cinar E, Saxena S, Uygur F. Combination therapy versus exercise and orthotic support in the management of pain in plantar fasciitis – a randomized controlled trial(external link) Foot Ankle Int. 2018;39(4):406–414
David JA, Sankarapandian V, Christopher PRH, et al. Steroid injections for painful soles of heels in adults(external link) Cochrane Review, 2017
Cinar E, Saxena S, Uygur F. Combination therapy versus exercise and orthotic support in the management of pain in plantar fasciitis – a randomized controlled trial(external link) Foot Ankle Int. 2018;39(4):406–414
Complete guide to plantar fasciitis(external link) PainScience.com, 2024. There's a cost to access the full book-length tutorial
Continuing professional development
Podcast
Rupesh Puna discusses foot pain throughout the lifespan. He uses a case-based approach highlighting 4 common conditions: Sever’s disease, Morton’s neuroma, plantar fasciitis and osteoarthritis of the foot.
 (external link)
(external link)
(Goodfellow Podcast, NZ, 2020)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Sara Jayne Pietersen, FRNZCGP, Auckland
Last reviewed:





