Methamphetamine addiction
Methamphetamine is also known as P, meth, ice, speed, pure, burn, goey, crank, crystal, ice, yaba and tina
Key points about methamphetamine addiction
- Methamphetamine is a strong and addictive drug.
- If you use it, you are at risk of becoming addicted.
- Long-term methamphetamine use harms your physical and mental health, relationships and emotional wellbeing.
- However, there are services that have helped many people to overcome this addiction.

Methamphetamine is a powerful, highly addictive stimulant drug that affects your central nervous system. It causes rapid release of the chemicals dopamine, serotonin and noradrenaline and this produces feelings of increased energy, mood and libido (sex drive). You may feel much more confident, alert and happy/euphoric (a 'high').
All drug use has a risk of harm, but methamphetamine is a particularly strong and addictive drug. People who use it can quickly become dependent on it. Read more about why methamphetamine is so addictive below.
Video: Did you know – methamphetamine
(NZ Drug Foundation, NZ 2024)
This video is also available in te reo Māori(external link).
How to recognise an overdose
| Overdose of methamphetamine can result in heart attack or stroke, and even death. Call 111 if you or someone else is experiencing these symptoms of overdose: | |
|
|
Addiction can harm your physical and mental health, as well as leading to losing your job, savings, home and relationships. You also risk overdose from a strong batch or large dose of methamphetamine, which can be fatal.
Addiction is a health condition, not a lifestyle choice or weakness. It’s important to get help sooner rather than later.
Thousands of New Zealanders have beaten their addiction to methamphetamine. There are many services that can help you to recover, from online counselling to inpatient rehab. Although relapse is normal during your recovery, expect to recover. Most people who have an addiction will recover.
The immediate response to using methamphetamine is a rush with increased heart rate, metabolism and blood pressure for up to 30 minutes.
Then the high – when you experience increased levels of energy and wellbeing – lasts for 4 to 16 hours. You can talk a lot and get into arguments. As the high begins to fade, the desire to continue it can lead to the uncontrolled use of more methamphetamine or alcohol. This is known as the binge. You can grind you teeth, pick at your skin and feel paranoid (fearful for no reason). Eventually you get no more high, despite repeated drug use, but this can take days to happen.
Towards the end of the binge comes a stage of called tweaking. It can be hard to sleep and you feel irritable, restless and paranoid. You may also get headaches and dizziness, hallucinations (seeing and hearing things that are not there) and confusion.
This is followed by a crash when your body shuts down and you need to sleep. It can last several days before you return to something like normal. However you’re likely to be starved, dehydrated and mentally, physically and emotionally exhausted.
Then withdrawal starts. You can feel anxious, have trouble sleeping and concentrating, feel sad or have mood swings, and get cravings. Because of this, people often take more methamphetamine to feel better. This can lead to a repetitive cycle of use, in which you use more methamphetamine more often. This makes it easy to become addicted to methamphetamine.
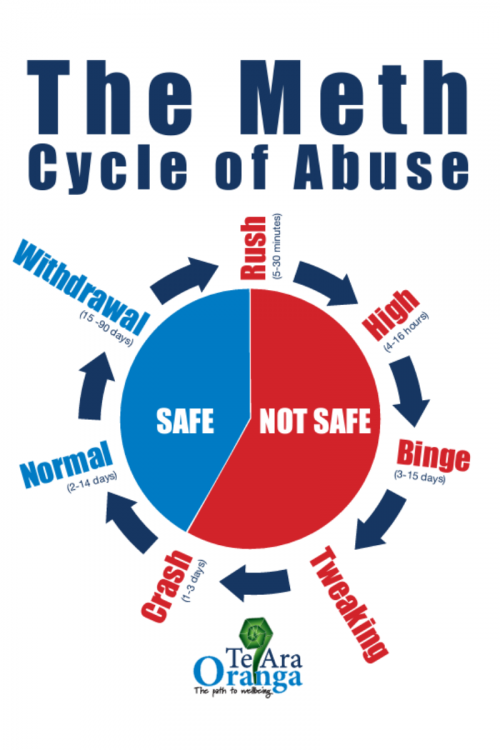
Image credit: Health New Zealand | Te Whatu Ora Te Tai Tokerau
Using methamphetamine is a risk to your physical and mental health. This is partly from the drug itself and partly from the things you tend to do when using it. Harm can also be caused by contaminants and by-products of the manufacturing process. This is particularly risky if you inject methamphetamine.
People who use methamphetamine over a long period of time may develop severe health problems such as:
- physical dependence, needing to use more meth to get the same effect and finding it difficult to stop, and experiencing withdrawal symptoms when you do
- ongoing sleep problems that affect your concentration, work, studies and quality of life
- decreased appetite and desire for food, resulting in weight loss and malnutrition, severe tooth decay, loss of teeth and skin sores
- severe mental and emotional symptoms, such as anxiety, mood changes, depression and suicidal thoughts, aggression and violent behaviour, psychosis (paranoia, hallucinations – seeing and hearing things that are not there – and delusions)
- cardiovascular problems, eg, high blood pressure, stroke, heart attack.
- the unknown effect methamphetamine has when it's mixed with other drugs or medications
- risky sexual behaviour that leads to STIs (sexually transmitted infections) or unplanned pregnancy
- risk of overdose from a strong batch or large dose of methamphetamine, which can be fatal
- risks of injecting (eg, hepatitis C, HIV/AIDS, skin infection, septicaemia).
You also risk losing your job, savings, home and relationships, and put yourself at risk of a criminal conviction. Methamphetamine is classified as a Class A drug, as is heroin.
While you may recover from some of the harm after you stop using the drug, some health effects may be permanent. The sooner you stop, the better the outlook for your long-term health.
Addiction means losing control over your use and finding it difficult to stop using it. Addiction includes feeling cravings and a compulsive drive to keep using, despite its bad effects. If you're addicted you can have a physical need for the drug or a psychological desire for it.
Watch out for the following 4 key 'Cs':
- compulsion
- loss of control
- cravings
- continued use despite the consequences.
If you've been using methamphetamine often, you might not notice how much it's affecting you. Ask someone you trust if they think it's harming you and your life.
You are likely to be addicted if you're:
- using more methamphetamine than you used to
- finding it hard to stop using
- missing school, work or family commitments
- always thinking about it.
If you’re not sure, test your drug use(external link) and learn more about when to find help for your drug use(external link).
Addiction gets worse over time, so if you notice the signs early, it's easier to stop at that point. The longer you're addicted, the harder it is to break free. Addiction can be treated with:
- counselling (online, by telephone or in person)
- motivational interviewing and cognitive behaviour therapy (types of psychological treatment that encourage you to change your behaviour)
- medication
- group therapy
- family therapy
- detox programs in hospital or at home
- residential treatment programmes (you can find a residential alcohol and other drug treatment service through this Healthpoint link(external link))
- rehab in hospital or at home.
No single treatment will work for everyone first time. You can talk to your doctor or other healthcare provider to make a treatment plan that suits you. Relapse is to be expected. Having a realistic plan that provides ongoing help for you and your family will help you avoid and/or get through relapses.
If you decide to cut back or stop after using methamphetamine often, you are likely to experience withdrawal symptoms. It’s a good idea to get some help when you do. Counselling and support from a healthcare provider, whānau and friends is the best approach to help you stop using methamphetamine.
- Tell your partner, close friends or family members that you want to stop using meth so they can support you to make the change. Read about tips for talking about your drug use.(external link)
- Contact one of the specialised services that know about how to stop using methamphetamine, such as the free Meth Help(external link) counselling service (call 0800 METH HELP or 0800 638 443) or the Alcohol and Drug Helpline(external link) (0800 787 797). See The Level(external link) for a list of other support services(external link).
- Talk to your doctor. If depression or anxiety is the underlying cause for your drug use, they may prescribe medication for that or to help you sleep during your withdrawal stage. If you have been using other drugs, eg, alcohol or benzodiazepines, tell your doctor as you may need specialist help (stopping these suddenly may be dangerous).
- Find a counsellor or therapist(external link) to talk to about your methamphetamine use and any other problems in your life that may have led you into using methamphetamine.
There are a lot of different things that will affect how long and intense your withdrawal will be. They include:
- what you have been using
- what else you have been using at the same time
- how much you have been using
- how often you have been using
- how long you have been using
- how you have been using (drinking, smoking, snorting, injecting)
- how healthy you are generally
- if you have any mental or physical health issues
- your attitude
- the support you get from family, whānau and friends.
Before you stop
- Organise support, such as friends or family/whanau, your GP or other healthcare provider, or a support organisation such as the Alcohol Drug Helpline (0800 787 797) or 0800 METH HELP.
- Organise a safe place, somewhere quiet where people aren’t using drugs.
- Plan ahead, including having a routine (getting up at a set time, showering, having breakfast and so on), things you enjoy doing and treats that help you to relax and avoid using.
- Work out a strategy for managing your cravings(external link), such as delaying the decision to use, distracting yourself with things to do, celebrate when you resist and using your breathing to calm yourself.
- Learn some strategies to help you sleep, such as having regular bedtimes, natural products that make you sleepy, keeping your bedroom for sleep.
Find more ideas in Te Pou's guide for people trying to reduce or stop using methamphetamine(external link).
Apps reviewed by Healthify
You may find it useful to look at some mental health and wellbeing apps.
It's safest to not use methamphetamine, but if you do use it, there are a few things you can do to reduce harm to yourself and others.
Being safer around methamphetamine
If you're going to use, before you do:
- make arrangements for children to be cared for by someone who is not using
- eat well for energy reserves
- clean your teeth
- use soap and water or alcohol swabs to clean your hands.
When using:
- use chewing gum to minimise tooth grinding
- sip water as your mouth will get dry, but not too much
- avoid alcohol and caffeinated drinks which dehydrate you
- avoid driving as your judgement will be impaired
- avoid mixing methamphetamine with other drugs or medications
- if you have sex, use condoms and lube and practice safe sex.
After using:
- catch up on fluids, food and sleep the next day
- avoid driving as you will be tired.
Method of use
Orally
If you're taking any type of speed, including methamphetamine, taking it orally is generally safer than smoking, injecting or snorting. This is because your stomach can handle acidic and foreign substances better than your lungs, veins or nose. Swallowing methamphetamine in empty pill capsules or wrapped in cigarette papers and drinking plenty of water reduces potential harm.
Smoking
The vapour produced from smoking methamphetamine can damage your lungs, and smoking is more addictive than snorting or eating. If you do smoke, use a shatterproof Pyrex pipe. Other pipes (or glass) can get too hot or give off toxic fumes. Avoid using broken or cracked pipes. Damaged pipes can lead to burns, cuts and infections.
Snorting
If you snort methamphetamine, make sure it's finely chopped with a razor or knife and use alternate nostrils. Also, avoid sharing straws for snorting. Blood and mucus left on the straw can cause the spread of blood-borne viruses, such as hepatitis and HIV.
Injecting
Injecting methamphetamine increases your risks of HIV, hepatitis and sepsis (a bacterial infection of your injecting wound), if you share needles and other equipment. There's also a risk of skin abscesses and collapsed veins. Using a wheel filter can help to remove impurities that cause infections. Injecting also increases your risk of stroke and heart attack.
If you are injecting, you can access needles, syringes and other equipment to support safe injecting practice and reduce risk of health-related complications through the Needle Exchange Programme(external link). Needle exchanges also provide for the safe disposal of used needles and syringes.
There are things you can do if you know someone who is using methamphetamine, and you’d like to support them to change their drug use.
- Consider ways to talk to them about their drug use. A good way is to bring up any changes you’ve noticed in things such as their appearance, appetite, sleep patterns, energy levels or levels of financial stress. Read more about tips on how to talk to someone about their drug use(external link).
- Be patient. Let them know you’re there to support them as much as you can. Encourage them to call a support service such as the Alcohol Drug Helpline (0800 787 797) or 0800 METH HELP.
- Help them through withdrawal. Read more about managing drug withdrawal(external link).
- Encourage healthy eating and provide healthy food options.
- Celebrate successes with them. These may be things such as eating well, exercising or having a drug-free day.
- Talk to them about what is motivating them to change their drug use and remind them of these things when they find things challenging.
- Take care of yourself(external link) so you have the energy to provide support. Family Drug Support(external link) provides support for whānau and friends of those using alcohol or other drugs.
Video: Did you know – methamphetamine
Video: Let's make a change
(Northland District Health Board, NZ, 2017)
Video: The cycle of meth abuse
(Northland District Health Board, NZ, 2017)
Video: Methamphetamine Patu i te hoarir
(Northland District Health Board, NZ, 2017)
Video: The road to recovery
(Northland District Health Board, NZ, 2017)
The following links provide further information about methamphetamine addiction. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
The Level(external link) is a website for people who use drugs, including methamphetamine(external link). It includes information to support you and your family/whānau if you want to make changes to your drug use(external link).
Managing withdrawal(external link) The Level, NZ
Kina Families and Addictions Trust(external link) Support for family, whānau and friends of people using alcohol and other drugs
Care NZ Manaaki Aotearoa(external link)
Cannabis, methamphetamine and oral health(external link) Health New Zealand | Te Whatu Ora
Methamphetamine and the law(external link) NZ Police
Apps
Mental health and wellbeing apps
Brochures
Methamphetamine(external link) Te Ara Oranga, NZ
Methamphetamine – P(external link) Community Alcohol and Drug Services, NZ
Talk about it – A guide to having open conversations about alcohol and other drugs with young people(external link) Alcohol and Drug Foundation, Australia
Living well – life strategies for family, whānau and friends of people using alcohol and other drugs(external link) Kina Families & Addictions Trust, NZ
P’d off – A guide for people trying to reduce or stop methamphetamine(external link) Te Pou, NZ
MethHelp – how to stay in control(external link) Drug Foundation NZ
Te Aka Mātua – basic drug information for mātua and concerned whānau(external link) Whare Tukutuku, NZ
A guide to talking therapies in NZ(external link) Te Pou, NZ
References
- Methamphetamine(external link) The Level, NZ
- Methamphetamine(external link) National Institute on Drug Abuse, US, 2024
- Methamphetamine(external link) Alcohol and Drug Helpline, NZ
- Addressing methamphetamine use in primary care(external link) BPAC, NZ, 2018
- Methamphetamine(external link) Te Ara Oranga, NZ
Treating methamphetamine addiction
- Health professionals need to be proactive when the opportunity arises in identifying people who have problems with methamphetamine use, as they may have little contact with health services and are unlikely to reveal their drug use without being asked.
- Methamphetamine use is most prevalent among people aged in their 30s and under, and is more common in males compared with females and in Māori compared to people of other ethnicities.
- People who use methamphetamine are at risk of dependency, psychosis and other mental and physical health complications, as well as financial, family, relationship and legal problems.
- Counselling and support from a health professional, friends and family is currently the best approach for helping people to stop using methamphetamine.
- Evidence does not support the use of any currently available pharmacological treatments to help patients quit or prevent relapses.
- There are a variety of self-help resources and support programmes available that patients can be directed to.
Read more: Addressing methamphetamine use in primary care(external link) BPAC, NZ, 2018
Guidelines
Substance withdrawal management – guidelines for medical and nursing practitioners(external link) Te Pou, NZ, 2019
Methamphetamine treatment guidelines(external link) Turning Point, Australia, 2018
Other information
Interventions and treatment for problematic use of methamphetamine and other amphetamine-type stimulants(external link) Matua Raki, NZ, 2010
Recognising and addressing the harmful mental health impacts of methamphetamine use(external link) The Royal Australian and New Zealand College of Psychiatrists, 2019
Mental health outcomes associated with of the use of amphetamines – a systematic review and meta-analysis(external link) EClinicalMedicine. 2019 Oct 17; 16:81–97
P'd off – A guide for people trying to reduce or stop using methamphetamine(external link) Te Pou, NZ, 2022
Te Aka Mātua – basic drug information for mātua and concerned whānau(external link) Whare Tukutuku, NZ, 2022
Brochures
Community Alcohol and Drug Services, NZ, 2016
Matua Raki, NZ, 2010
Drug Foundation NZ, 2018
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Alistair Dunn, addiction specialist lead clinician, Opiate Substitution Treatment Service, Health New Zealand | Te Whatu Ora Te Tai Tokerau
Last reviewed:





