Frailty
Key points about frailty
- Frailty means your body has a harder time recovering from illness or injury. If you're frail, it takes longer to feel better after being unwell.
- People can be mildly, moderately, or severely frail.
- Frailty is more common as we get older, but younger people can also be frail due to health conditions, treatments, or life challenges.
- Sometimes frailty is caused by a health problem and sometimes being frail can lead to new health problems.
- The best way to manage frailty is to spot it early and make a care plan that fits your needs.

Frailty means you have a harder time getting better (bouncing back) after being unwell or injured. Frailty can affect many parts of your life, including:
- how well you can manage everyday tasks and take care of yourself
- your physical health and strength
- how easily you can move around
- your mood and emotional wellbeing
- how well you can manage living independently.

Image credit: Healthify He Puna Waiora
Being frail makes you more likely to become unwell and struggle with stressful situations, and this puts you at higher risk of poor health. Even small things, such as a mild infection, constipation, or a new medicine, can have a big impact. Bigger events, such as surgery, can be even harder to recover from. That’s why frailty should be treated like a long-term condition. If it’s not managed well, it can lead to more health problems.
Having long-term health conditions such as arthritis, COPD, kidney or liver disease increases your risk of frailty. Although it's more common in older adults, frailty can affect younger people too.
Just because you’re older doesn’t mean you will be frail. Frailty can be mild, moderate or severe – and your level of frailty can change over time. It may begin with small changes in your daily living that can slowly lead to bigger health problems. Frailty can be reversed, especially if it's picked up early. How well you recover depends on how severe it is and your overall health. You can lower your risk of frailty getting worse by noticing the signs early and getting the right support and care for your needs.
Video: Frailty – every step you take matters!
The diagnosis of frailty is complex. There are many different things that are looked at to understand if a person is frail. These include your health conditions, weight and how well you can move and take care of yourself. Some assessment tools have been developed to help healthcare providers decide whether someone is frail. Examples are the Rockwood Clinical Frailty Score(external link) and the Edmonton Frail Scale(external link).
When deciding if you are frail your healthcare provider may look at:
- your health conditions
- how fast you walk
- how active you are
- how strong your grip is
- your energy levels
- how independent you are, such as if you need help with your daily activities
- your weight, especially if you have lost weight without trying
- your blood test results.
After looking at different signs of frailty, you may be described as:
- Not frail if you’re doing well and recovering normally.
- Pre-frail if you’re starting to show some signs of frailty.
- Frail if you have several signs and may need extra support.
There are different levels of frailty as well, you may be mildly, moderately or severely frail.
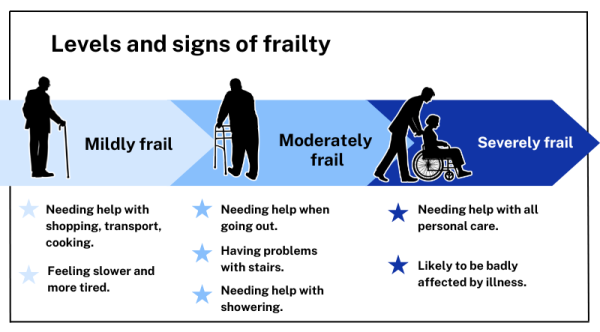
Image credit: Healthify He Puna Waiora (Based on the Rockwood Clinical Frailty Scale(external link))
Diagnosis helps identify people who are more likely to have serious health problems. Once frailty is identified, the right care and support can be put in place to help prevent those problems. If you are diagnosed with frailty it may affect the decisions your healthcare team makes about your care. This could include what tests or treatments are best for you, based on your overall health and how you might recover.
Older people with frailty are at higher risk of:
- falling
- being less able to move around
- bladder or bowel problems (incontinence)
- feeling confused or disoriented
- needing care in a rest home or care facility
- having side effects from new medicines
- a big decline in health due to a minor problem such as a mild infection.
Younger people with frailty are at higher risk of:
- not living as long
- having to go to hospital when they're unwell.
In some cases, frailty can improve. Depending on the cause, research shows that some people can move from being more frail to less frail with the right care and support. For some people frailty can’t be reversed, but taking care of yourself and managing your health can help you stay stable or slow down the progression of frailty.
Frailty can be caused by a health problem and can cause more health problems. For example, if you have a fall it may affect your muscle strength and mobility, causing frailty. On the other hand, if you have frailty, you may be more likely to fall.
However, although frailty is most commonly thought of as applying to older adults, younger people can also be frail for various reasons.
Risk factors for frailty include:
- falling
- older age
- being female
- chronic health conditions such as COPD, multiple sclerosis, ME/CFS, diabetes, stroke, heart disease or depression
- living in a low-income area
- having less education
- smoking
- being very overweight
- not getting enough nutrition (malnutrition)
- being Māori or Pasifika
- experiencing stress or trauma during childhood.
The key to managing frailty is noticing it early and developing a good care plan. This helps your healthcare team make better decisions which may reduce the impact of frailty on your health.
Your healthcare team may help manage frailty by:
- checking your medicines regularly to remove any you no longer need and reduce the risk of side effects from taking too many – this is called polypharmacy
- doing regular health check-ups, including both physical and mental health
- treating causes of weight loss and tiredness, such as depression, low iron (anaemia) or vitamin B12 deficiency
- offering a physical activity plan, including strength-building exercises (resistance training)
- assessing your care and support needs to make sure you get the right help
- reviewing your home environment to reduce your risk of falls
- talking with you about an advance care plan in case you become unwell or fall
- supporting healthy lifestyle choices, such as eating well, staying active, and not smoking.
There are things you can do to help lower your risk of frailty or stop it from getting worse.
- Stay active – exercise to improve your muscle strength and balance. Find out about green prescriptions or exercise groups in your area(external link).
- Eat a healthy balanced diet, making sure you get enough protein. If needed, nutritional supplements such as Ensure, Fortisip or vitamin D may be recommended. Talk to your doctor or nurse, they can help you with your diet and refer you to a dietitian if needed.
- Avoid smoking and if you drink alcohol, drink less.
- Get regular health check-ups including checking your hearing and eyesight.
- Keep your vaccines up to date.
- Stay connected. Spend time with whānau and friends, join a support group or an interest group.
- Think about getting a personal medical alarm.
Watch for signs of frailty. If you feel weaker, lose weight without trying, get tired easily or find it harder to move or care for yourself, talk to your healthcare provider. They can help you stay as healthy and independent as possible.
Apps reviewed by Healthify
You may find it useful to look at some falls prevention apps, healthy ageing and wellness apps, and joint and bone health apps.
Below are some support services and information designed to meet the needs of older people.
- Age Concern NZ(external link) works to promote the rights, quality of life and wellbeing of older people around New Zealand.
- Carers New Zealand(external link) is a national information centre for family carers who support frail older family members or friends.
- Eldernet New Zealand(external link) provides comprehensive, up-to-date information about services available for older people (eg, home help services, respite care, residential care, dementia care and community groups).
- Hub of Hope NZ(external link) is a non-profit organisation that equips and mobilises caring people to provide spiritual support for those at the end of their lives and their whanau.
- Live Stronger for Longer(external link) provides information for older people and their carers about preventing falls and fractures (funded by ACC, Health New Zealand | Te Whatu Ora and Health Quality & Safety Commission).
- New Zealand Home and Community Health Association(external link) provides information on available home health care services.
- Seniorline(external link) is a national service for older people who are considering rest home or long stay hospital care, or who are already in care.
- Sorted(external link) provides information on managing your money and moving into a rest home or retirement village. Its living in retirement(external link) section provides you with information in your semi-retired/retired years and how best to manage your nest egg.
- SuperGold Card(external link) is a discounts and concessions card issued free to all eligible seniors and veterans.
Read more about services for older people.
Live stronger for longer(external link) NZ
Brochures
Sample meal plan for frail older people [PDF, 102 KB]Ministry of Health, NZ, 2013
Physical activity for older people (65+)(external link) Ministry of Health, NZ, 2013
Frailty(external link) NHS, UK
Apps
Falls prevention apps
Healthy ageing and wellness apps
Joint and bone health apps
References
- Defining and recognising frailty(external link) Health Quality & Safety Commission, NZ, 2019
- Health and frailty assessment for older adults(external link) Auckland Regional HealthPathways, NZ, 2019
- Frailty in older people – a discussion(external link) BPAC, NZ, 2018
- Allison R 2nd, Assadzandi S, Adelman M. Frailty – evaluation and management(external link) Am Fam Physician 2021;103(4):219–226
- Bai G, Wang Y, Mak JKL, et al. Is frailty different in younger adults compared to old? Prevalence, characteristics, and risk factors of early-life and late-life frailty in samples from Sweden and UK(external link) Gerontology 2023;69(12):1385–1393Won CW. Diagnosis and management of frailty in primary health care Korean J Fam Med. 2020;41(4):207–213
- Frailty(external link) Department of Health, Victoria, Australia, 2024
- Introduction to frailty(external link) British Geriatrics Society, UK, 2014
Clinical resources and guidelines
The HQSC frailty care guides(external link) HQSC, NZ, 2023 are a suite of 26 nursing decision support tools covering the spectrum of frailty from deterioration to communication and advance treatment planning.
Clinical Frailty Scale
Other resources
Frailty in older people – a discussion(external link) BPAC, NZ, 2018
Management of multimorbidity(external link) Health New Zealand | Te Whatu Ora
Continuing professional development
Maximising the health of older people – Goodfellow MedTalk(external link) (Goodfellow MedTalks, NZ, 2018)
Dr Helen Fulcher, Goodfellow GP advisor, talks with University of Auckland Head of School of Population Health and general practitioner Professor Ngaire Kerse about maximising the health of older patients.
Optimisation of care of older patients(external link) Podcast Goodfellow NZ, 2018
Lucy Fergus talks about optimisation of care in older patients. Lucy is a geriatrician and medical director for older person’s health, rehabilitation and allied services at Hawkes Bay Hospital.
The impact of frailty on prescribing medication – Goodfellow webinar(external link)
Dr Chris Cameron, a general physician and clinical pharmacologist in Wellington, discusses what defines frailty and why this is important to assess in older patients. Frailty can be used as a starting point to review and withdraw medicines, as it can give us an indication of the length of life left.
Frail patients – Goodfellow webinar(external link)
Geriatrician and General Physician Helen Kenealy discusses frailty, including what frailty is, its prevalence in New Zealand, risk factors, presentation, measurement, and the importance of assessing it. Helen will also discuss practical tools for assessing frailty, adverse outcomes, and effective management strategies.
Brochures

Ministry of Health, NZ, 2013

Frailty NHS, UK
Ministry of Health, NZ, 2013
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Catherine Mounsey, Nurse Practitioner Older Adults, Bay of Plenty; Rosie Winters, Nurse Practitioner Older Adults, Bay of Plenty
Last reviewed:





