If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Fibroids
Key points about fibroids
- Fibroids are non-cancerous growths in the muscle wall of your uterus.
- They’re common and usually develop during your reproductive years. They tend to get smaller after menopause.
- Most are small and don’t cause any symptoms, but if they’re large and in certain areas of your uterus they can cause heavy bleeding and pain.
- Treatment depends on the type, size, number and location of your fibroids.

Fibroids are benign (non-cancerous) growths in the muscle wall of your uterus (womb).
They can grow anywhere in your uterus, and vary in size from as small as a pea to as large as a melon. They can grow on the outer wall of the muscle, within the muscle wall, or on the inner wall lining your uterus.
Fibroids are common and usually develop during your reproductive years. They tend to get smaller after menopause.
Most are small and don’t cause any symptoms or only mild symptoms. However, if they’re large and in certain areas of your uterus they can cause heavy bleeding and pain. Treatments are available depending on the type, size, number and location of your fibroids.
It’s not known what causes fibroids, but their growth is linked to the hormones oestrogen and progesterone.
They usually develop during your reproductive years when oestrogen levels are at their highest, and tend to shrink when oestrogen levels reduce, such as after menopause.
Things that increase the risk of fibroids include:
- being in your later reproductive years (35 years and over)
- starting your periods early
- having never been pregnant
- being overweight or obese
- having a family history of fibroids.
Fibroids can be grouped according to where they grow in your uterus (womb).
The main types of fibroids are:
- intramural fibroids – these develop in the muscle wall of your uterus and are the most common type
- subserosal fibroids – these grow on the outside surface of your uterus and can be very large
- submucosal fibroids – these develop in the inside surface of your uterus and grow into the cavity of your uterus.
Sometimes, subserosal or submucosal fibroids are attached to the uterus by a stalk of tissue. These are called pedunculated fibroids.
The image below shows the different types of fibroids.
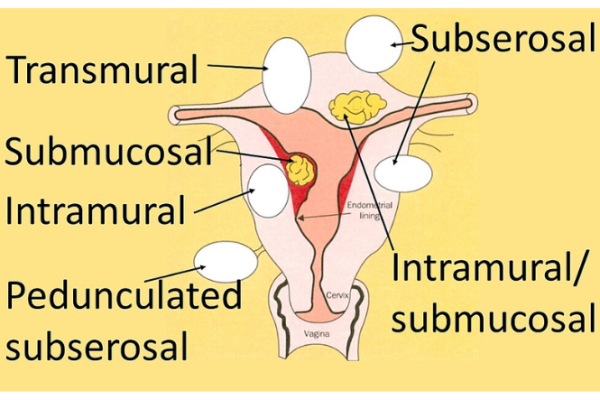
Image credit: Mikael Häggström via Wikimedia Commons (external link)
If you have fibroids you may have:
- heavy periods (heavy menstrual bleeding)
- abdominal (tummy) pain or a swollen tummy
- pelvic pain
- pain during sex
- a need to urinate (pee) more often, if a fibroid is pressing on your bladder
- constipation (hard poo, difficulty passing poo), if a fibroid is pressing on your bowel.
Symptoms depend on how many fibroids you have, their size and where they are. You may have iron deficiency due to heavy periods and this may make you feel tired or dizzy.
For most people, fibroids don’t usually cause problems with pregnancy or getting pregnant.
Your healthcare provider will ask you about your symptoms and do a pelvic (internal) exam.
Other tests you may have include:
- an ultrasound scan – this may be done on the outside of your tummy or internally with a small probe inserted into your vagina
- an MRI scan – a special imaging test that creates detailed pictures and may be recommended by a specialist in specific situations
- a hysteroscopy – where a small telescope is inserted through your vagina and cervix to look inside your uterus
- a laparoscopy – where a small cut is made through your abdomen which allows a small telescope to be inserted to see your pelvic organs.
In some cases, a biopsy may be taken for closer examination. This is where a small sample of tissue is removed during a hysteroscopy.
Fibroids don’t need to be treated if they’re not causing any symptoms, and they tend to shrink by themselves after you reach menopause.
If you do have symptoms, treatment depends on:
- the type, size, number and location of the fibroids
- how bad your symptoms are
- how much your symptoms affect your quality of life
- your age and how close you are to menopause
- whether you might want to become pregnant in the future.
Medicines to treat symptoms
If you do have symptoms caused by fibroids, such as heavy bleeding, medicines will usually be recommended. However, they may not work well if you have large fibroids.
These medicines include:
- tranexamic acid to decrease bleeding
- anti-inflammatory medicines, such as ibuprofen or mefenamic acid (Ponstan) for heavy painful periods
- hormonal treatments such as an oral contraceptive pill or progesterone only medication such as medroxyprogesterone acetate (Provera)
- a hormonal intrauterine contraceptive device (IUD) such as a Mirena if you have small fibroids that don’t grow into your uterus
- gonadotropin-releasing hormone (GnRH) agonists such as goserelin to stop periods for a while and shrink fibroids – they may be used before surgery to reduce bleeding.
Surgery to remove fibroids
Surgery to remove your fibroids may be considered if your symptoms are very severe and medicines aren’t working well. A specialist doctor can discuss which option is best for you.
Types of surgery to remove fibroids
- Hysteroscopic resection – where a small telescope and small surgical devices are inserted through your vagina and cervix into your uterus to remove fibroids inside the uterus. It’s suitable if you want to have children in the future.
- Myomectomy – an operation to remove fibroids from the wall of your uterus. It’s an alternative to hysterectomy (removal of your uterus) if you still wish to have children, but it’s not suitable for all types of fibroids.
- Hysterectomy – an operation to remove your uterus. It may be recommended if you have large fibroids or severe bleeding and you don’t want to have any more children. Read more about hysterectomy.
Other treatments
Fibroid embolisation is an alternative to hysterectomy or myomectomy and may be recommended if you have large fibroids. It’s done under local anaesthetic by a radiologist (a doctor who specializes in X-rays). It involves using X-ray to guide a thin tube into the artery that supplies the fibroids and injecting a solution that blocks the artery causing the fibroid to shrink.
Making healthy lifestyle choices may help shrink fibroids or reduce your risk of getting fibroids.
- Try to stay at a healthy bodyweight.
- Keep physically active.
- Get your blood pressure checked regularly. A recent study suggests a possible link between high blood pressure and the development of fibroids.
- Eating a healthy diet with plenty of fruits, vegetables and wholegrains will support your overall hormonal health and body weight.
Natural remedies may or may not help. Talk to your healthcare provider before taking any natural remedies or supplements.
See our page on heavy periods for self-care tips if you have heavy menstrual bleeding.
Symptoms usually improve with treatment or after menopause when fibroids often shrink. See your healthcare provider if you continue having symptoms or if you have new bleeding or other problems.
If you don’t need treatment because your fibroids aren’t causing problems, your healthcare provider may discuss whether monitoring is appropriate.
Problems with getting pregnant aren’t common if you have fibroids but see your healthcare provider if you’re having difficulty getting pregnant.
Fibroids(external link) Health New Zealand | Te Whatu Ora, NZ, 2025
Fibroid embolisation(external link) Health New Zealand | Te Whatu Ora, NZ, 2025
Brochures
Fibroids(external link) The Royal Women’s Hospital, Victoria, Australia, 2018
Myomectomy(external link) The Royal Women’s Hospital, Victoria, Australia, 2018
References
- Fibroids(external link) The Royal Women’s Hospital, Victoria, Australia, 2018
- Fibroids(external link) Patient Info, UK, 2023
- Fibroids(external link) NHS, UK, 2022
- How to treat uterine fibroids yourself(external link) Healthline, US, 2023
- Mitro SD, Wise LA, Waetjen LE, et al. Hypertension, cardiovascular risk factors, and uterine fibroid diagnosis in midlife(external link) JAMA Netw Open. 2024 Apr 16;7(4):e246832
- de Smit NS, de Lange ME, Boomsma MF, et al. Current treatment for symptomatic uterine fibroids – available evidence and therapeutic dilemmas(external link) The Lancet 2025;406(10498):91–102
- Uterine fibroids – patient-centred management starts with GPs(external link) NZ Doctor, 2024
- Uterine fibroids – effects fertility, perimenopause, menopause and beyond(external link) Goodfellow Unit Webinar, NZ, 2021
de Smit NS, de Lange ME, Boomsma MF, et al. Current treatment for symptomatic uterine fibroids – available evidence and therapeutic dilemmas(external link) The Lancet 2025;406(10498):91–102
Uterine fibroids – patient-centred management starts with GPs(external link) NZ Doctor, 2024
Uterine fibroids(external link) BMJ Best Practice, UK, 2025
Heavy menstrual bleeding – assessment and management(external link) NICE, UK, 2018 (updated 2021)
Uterine artery embolisation for the treatment of uterine fibroids(external link) RANZCOG, Australia and NZ, 2008 (reviewed 2020)
Fibroids in infertility(external link) RANZCOG, Australia and NZ, 2018
Mitro SD, Wise LA, Waetjen LE, et al. Hypertension, cardiovascular risk factors, and uterine fibroid diagnosis in midlife(external link) JAMA Netw Open 2024 Apr 16;7(4):e246832
Webinar
Uterine fibroids – effects fertility, perimenopause, menopause and beyond(external link) Goodfellow Unit Webinar, NZ, 2021
Podcast
Fibroids(external link) Dr Jessica Dunning, Goodfellow Unit, NZ, 2025 (Duration 28:38)
Credits: Healthify editorial team. Healthify is brought to you by health Navigator CharitableTrust
Reviewed by: Dr Grace Lee, FRNZCGP and Clinical Educator
Last reviewed:





