You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Emphysema
Key points about emphysema
- Emphysema is a form of COPD (chronic obstructive pulmonary disease) along with chronic bronchitis and asthma.
- It's a lung condition causing shortness of breath and a persistent cough. It's often caused by smoking or significant long-term exposure to dust.
- Emphysema happens when your lungs get damaged making it harder to absorb enough oxygen into your bloodstream when you breathe.
- The damage can’t be reversed or 'fixed', but there are treatments and things you can do to improve your breathing. Medicines may help relieve your symptoms.
- Avoiding all potential lung irritants, including vaping and smoking,is important.

Emphysema happens when the air sacs (alveoli) in your lungs get damaged and are eventually destroyed. This is similar to a deciduous tree losing its leaves in autumn or earlier in unfavourable conditions. This decreases your lung capacity and makes it harder to absorb enough oxygen into the blood stream when you breathe.
It's usually caused by smoking or being exposed to a lot of dust over your life-time.
Smoking has been the most common cause of emphysema, although more than a quarter of people with this condition may never have smoked but may have been exposed to an irritating level of dust.
Other possible causes of emphysema include:
- air pollutants in the home and workplace
- alpha-1 antitrypsin deficiency, a genetic (inherited) factor
- respiratory infections.
Cigarette smoking or dust exposure and air pollution may not only destroy lung tissue, it will also irritate your airway. This causes inflammation and damage to the linings of the bronchial tubes. It results in swollen airways, mucus production and difficulty clearing the airways. All of these changes can lead to shortness of breath or wheezing and cough which are the other symptoms of COPD and chronic bronchitis.
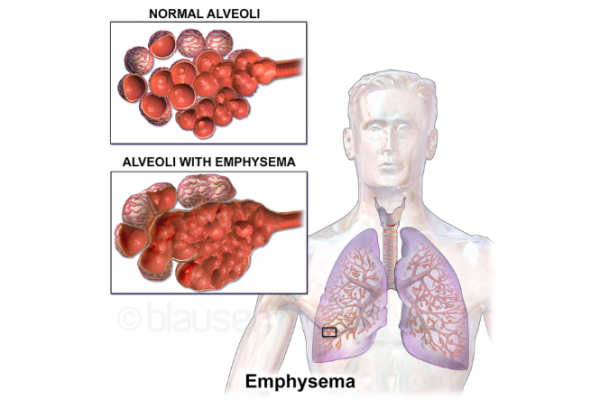
Image credit: Blausen Medical Communications, Inc.(external link) Wikimedia Commons
The main symptoms are:
- being short of breath
- having a chronic cough, eg, a "smoker's" cough for some people
- longer than usual out-breaths and possibly wheezing
- more rapid breathing
- finding it hard to breathe even when you're sitting or lying down.
The diagnosis of emphysema or COPD can't be made solely on symptoms. Several tests are used to make the diagnosis, such as:
- A breathing test, called spirometry. Depending on where you live, this may be done at your local medical centre but may need a referral. For some people this may still be normal as spirometry only picks up 'wheezy lungs' as part of COPD. Additional breathing tests are then needed.
- Blood tests are generally only useful if you have a family history of alpha-1 antitrypsin deficiency or if there is a concern about asthma.
- A chest X-ray is important for ruling out other lung conditions. It's not a good way to diagnose emphysema or COPD.
- A CT scan will pick up or diagnose emphysema. You will need a special referral from your healthcare provider and it may not be freely available locally.
A spirometry is the basic and most useful test. Often this needs a referral to a hospital clinic as many GPs don’t do this test. Some people need to have more extensive hospital-based “full” lung testing in a respiratory specialist clinic.
Avoid irritants
The number one treatment is to quit smoking (if you smoke). Avoiding anything that irritates your lungs and airway is also very important. This includes avoiding vaping, and having ongoing lung infections treated.
Medicines
You may also be prescribed inhaler medicines to open your airways and medicine to prevent or treat infections. There are many different types of medicines used for COPD conditions such as emphysema. Read more about medicines for COPD.
Exercise
Daily exercise is one of the most important ways to clear your air tubes of phlegm and to keep your breathing as efficient as possible. Your healthcare provider may also ask you to do special exercises to improve your breathing, and refer you to a special programme called pulmonary rehabilitation.
There are important things you can do to help you breathe more easily and lessen the chance of a flare-up or exacerbation (your symptoms suddenly getting worse).
- Quit smoking and avoid inhaling irritating dusts and chemicals.
- Have a COPD action plan(external link) (versions in other languages are linked in the more information section below).
- Stay active and ideally exercise for at least 20 to 30 minutes daily, but within your limitations. “Huffing and puffing” is okay as long as it's within your control. Read more about exercises at home for COPD(external link).
- Improve the way you breathe, you may need to learn breathing techniques(external link).
- Attend a pulmonary rehabilitation programme.
- Get your vaccinations, eg, the regular COVID-19 booster, the annual influenza vaccination and your 10-yearly whooping cough (and tetanus) booster. You should also consider the pneumococcal and the RSV vaccination although those are not generally funded.
- If you've been prescribed medicines, use them correctly. Inhalers may or may not be effective but this should be tested.
Read more about self-care measures.
Apps reviewed by Healthify
You may find it useful to look at some Quit smoking apps, COPD apps and Breathing apps.
It can be distressing and frustrating to have breathing difficulties. Get help or find support when things are tough. Ask your healthcare provider about local support groups for COPD in your area. For more support services, see support services for COPD.
Emphysema(external link) Health Direct, Australia
What is COPD?(external link) Asthma + Respiratory Foundation, NZ
COPD and smoking(external link) Centre for Disease Control and Prevention, US
COPD – the essentials(external link) NHS Choices, UK
Emphysema(external link) Buteyko Breathing can be helpful for some people but shouldn't replace medicines if they've been prescribed and are working well
Brochures
Breathlessness strategies for COPD(external link) Asthma + Respiratory Foundation NZ
COPD action plan(external link) Asthma + Respiratory NZ te reo Māori(external link), Samoan(external link), Tongan(external link), Chinese simplified(external link)
Home exercises for COPD(external link) Asthma + Respiratory Foundation NZ
Apps
Quit smoking apps
COPD apps
Breathing apps
References
- Hancox RJ, Jones S, Baggott C, Chen D et al. on behalf of the Asthma and Respiratory Foundation NZ 2021 COPD guidelines – quick reference guide(external link)
- Tamondong-Lachica DR, Skolnik N, Hust JR, et al. GOLD 2023 update – implications for clinical practice(external link) Int J Chron Obstruct Pulm Dis. 2023;18:745–54
- Yang IA, George J, McDonald CF, et al. The COPD-X plan – Australian and New Zealand guidelines for the management of COPD 2024(external link) Version 2.75, June 2024
- Pahal P, Avula A, Sharma S. Stat Pearls Emphysema(external link) NIH National Library of Medicine, Update January 2023
- Yang IA, Jenkins CR, Salvi SS. COPD in never-smokers – risk factors, pathogenesis and implications for prevention and treatment(external link) Lancet Resp 2022;10:497–511
- COPD and Vaping(external link) WedMD, US, 2024
Brochures
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Roland Meyer, Specialist Physician, Respiratory and General Medicine
Last reviewed: