Diverticular disease and diverticulitis | Pūtautau i te whēkau
Key points about diverticular disease and diverticulitis
- Diverticular disease (pūtautau i te whēkau) is a condition where small pockets or pouches (diverticula) form in the wall of your bowel, usually in your large intestine.
- These pouches can remain trouble-free or they can become inflamed, causing pain and constipation.
- They become inflamed when undigested food, or bacteria, becomes trapped inside them – a condition we call diverticulitis.
- Having diverticula is very common, occurring in about half of all people over 60 years of age.

Diverticulosis
Diverticulosis is a common condition where small pouches or pockets, known as diverticula, form in the wall of your colon or large intestine. These pouches can develop over time, typically as you get older. Your large intestine becomes weaker with age, and the pressure of hard stools (poo) passing through it is thought to cause the bulges to form. They are usually harmless and may not cause any symptoms. Many people with diverticulosis don't even know they have it.
Diverticulitis
Diverticulitis occurs when 1 or more of these diverticula become inflamed or infected. This can cause various symptoms, eg, abdominal pain, fever, and changes in bowel habits. In severe cases, diverticulitis can lead to complications like abscesses (collections of infection), bowel obstructions, perforations (holes in the bowel wall) and bleeding.
The image below shows the location of the colon and diverticula in the colon wall.
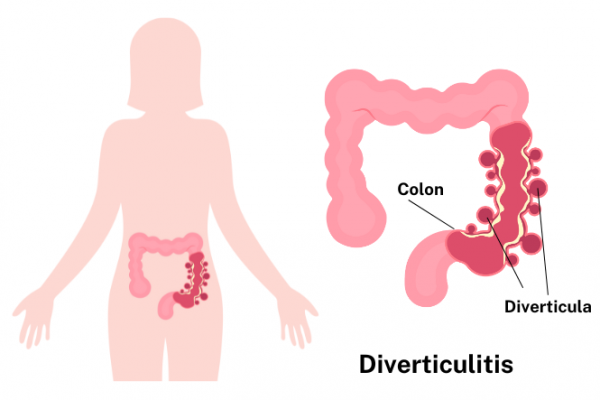
Image credit: Healthify and Canva
Diverticulosis
Most people with diverticulosis don't have symptoms at all. Sometimes it causes mild cramps, bloating or constipation. Diverticulosis is often found through tests ordered for something else. For example, it's often found during a colonoscopy to screen for cancer. A high-fibre diet and mild pain reliever will often relieve symptoms.
If the pouches become inflamed or infected, you have a condition called diverticulitis.
Diverticulitis
The most common symptom of diverticulitis is abdominal pain, usually on the left side. You may also have:
- fever
- nausea (feeling sick)
- vomiting (being sick)
- chills
- cramping
- constipation.
In serious cases, diverticulitis can lead to bleeding, tears, or blockages.
Note: If you have pain, fever and chills, or bleeding, this can be serious and you should seek medical treatment immediately.
Diverticulosis is often diagnosed during tests, eg, a colonoscopy, where a small camera is passed up your back passage, through which a doctor can see inside your bowel and examine the bowel wall.
Sometimes, instead of using a camera, air and contrast material are passed into your large bowel to outline the bowel wall and a CT scan of the bowel is done. This kind of test is called CT colonography.
Diverticulitis can often be diagnosed using regular CT scans or, less commonly, ultrasound of the bowel. Sometimes though, doctors can diagnose and treat someone for diverticulitis just based on their history, physical exam and blood tests showing inflammation or infection.
Diverticulosis
Treatment for diverticular disease depends on how severe your symptoms are.
People with bowel pouches, which haven't become inflamed, generally only require a change in diet to improve their condition. The diet must include good quantities of roughage. At least 5 servings of fruit and vegetables a day should be eaten (a serving is roughly the size of your cupped hand). Fibrous fruits such as apples and pears are best, along with fresh fruits, vegetables and whole grain cereals.
Increasing the fibre in your diet may cause wind and abdominal pain for a few weeks. This is caused by the bowel adjusting to the change in eating habits. Increase the fibre gradually to minimise this problem.
It can be helpful to visit a dietitian after being diagnosed with diverticular disease to go through what foods are best for you.
Diverticulitis
When the bowel pouches have become inflamed (diverticulitis), treatment is aimed at resting your bowel, relieving pain and fighting infection. At this stage, a low-fibre, or fluid only diet, is recommended to rest your bowel.
- On a low-fibre diet, it's important to prevent constipation and laxatives are prescribed to do this.
- Bowel spasms can be painful when the pouches are inflamed – painkillers or anti-spasmodic tablets are prescribed to help.
- In many cases, uncomplicated diverticulitis is caused by inflammation rather than infection. Therefore antibiotics are sometimes not needed if you don't have a fever or blood tests suggesting you have an infection. If your healthcare provider suspects infection, antibiotics are usually prescribed and can often be taken at home. However, sometimes you may need to go to hospital if you're very unwell or your symptoms aren't getting better.
Rarely, surgery needs to be performed to remove affected parts of the bowel.
Probiotics
Although more research is needed, research suggests probiotics may help treat the symptoms of diverticulosis, prevent the onset of diverticulitis, and reduce the chance of recurrent symptoms. Probiotics are live bacteria, like those normally found in your gastrointestinal tract (GI tract). Probiotics can be found in dietary supplements – in capsules, tablets, and powders – and in some foods, eg, yoghurt.
Diverticular disease(external link) National Institute of Diabetes and Digestive and Kidney Diseases, US
Diverticular disease and diverticulitis(external link) NHS Choices, UK
Diverticulosis, diverticular disease, diverticulitis(external link) Patient Info, UK
Apps
Resources
Eating guidelines for diverticulosis, diverticular disease and diverticulitis(external link) HealthInfo, NZ
References
- Antibiotics – choices for common infections(external link) BPAC, NZ, 2017(external link)
- Diverticular disease(external link) Auckland Regional HealthPathways, NZ, 2017
Information, guidelines and reviews
It is thought that in many cases, uncomplicated diverticulitis is caused by inflammatory processes, rather than infection. Therefore antibiotic treatment is not routinely required, but it may be considered if the patient’s symptoms persist or worsen despite dietary management and analgesia. If needed, prescribe trimethoprim + sulfamethoxazole 960 mg, 2 times daily, with metronidazole, 400 mg, 3 times daily, for 5 days. Antibiotics – choices for common infections(external link) BPAC, NZ, 2017
Diverticular disease – diagnosis and management(external link) NICE Guideline, No. 147, UK, 2019
Diverticulitis: pockets of knowledge(external link) B-QuiCK BPAC, NZ
Continuing professional development
Dr Nagham Al Mozany - General and Colorectal Surgeon - 2019 Goodfellow Symposium v2
Dr Nagham Al Mozany talks about key take-home messages for diverticular disease in the Goodfellow Symposium 2019. This video may take a few moments to load.
(Mobile Health NZ, 2019)
Apps
Credits: Written by Anna Mickell RCpN.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:





