You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Breast cancer – after treatment
Key points about what can happen after breast cancer treatment
- Following breast cancer treatment, it's natural to have questions and concerns that reach beyond simply whether the initial cancer has been cured.
- Experiencing breast cancer can affect you physically, emotionally and psychologically.
- It's important to reach out for advice and support hen you need it.
- This page provides information about common concerns and what you can do.

Following breast cancer treatment, it's natural to have questions and concerns that reach beyond simply whether the initial cancer has been cured.
Experiencing breast cancer can affect you physically, emotionally and psychologically. It's important to reach out for advice and support when you need it. This may be after your treatment is completed.
Regular health checks are recommended for people who have had breast cancer, and follow-up is advised for 10 years – usually starting on a 3-monthly basis. Your healthcare team will provide information on your ongoing care, and will be able to give advice and direct you to helpful resources.
Surgery for breast cancer is usually less extensive today than it used to be. However, pain after surgery, radiation treatment or chemotherapy is still a reality for some people. Pain is not something you should ignore (even if it's possible for you to just carry on). Pain doesn't help your recovery and it can mean that it's harder to do the things that do help you to recover (eg, sleep and exercise).
There are ways to minimise pain, not all of which involve medicines. Your healthcare provider or pain clinic can suggest suitable options (eg, a programme of exercise, yoga, meditation or acupuncture). Low doses of certain antidepressant medications may be an option as they can ease some types of pain due to nerve irritation.
Numbness or tingling in your arm is more common if lymph nodes have been removed from your armpit. This occurs due to nerve damage in the area. It may improve over time as the nerves slowly regrow. However, it doesn't always improve and the numbness may be permanent. It's important to protect these numb areas from injury (eg, sunburn, sharp objects). If the numbness or tingling doesn't clear up in a few weeks or months you should talk to your healthcare provider.
During your recovery from surgery, it's possible for a fluid collection to build up over your chest or under your armpit – this is called a seroma. If the seroma is large and uncomfortable, sometimes fluid can be removed using a syringe. This may need to be repeated to help the seroma to resolve.
If the cancer, surgery or radiation treatment involved the lymph nodes in your armpit, the normal drainage of fluid (lymph) from your hand and arm back to your body may be affected. For some people, this can cause arm swelling (lymphoedema), but it's less common with today's treatments. If you notice swelling in your arm, talk to your healthcare provider and they may be able to refer you to a lymphoedema specialist.
When this is a risk, it can often be prevented by regaining movement in the shoulder and by carrying out regular arm exercises recommended by your breast-care nurse. It's important that you continue to protect this arm from injury, infection and sunburn and don't use it for heavy lifting. The problem can develop months or years after treatment.
These are well-known problems when recovering from breast cancer. In the past, you would have been advised to rest. Now, research shows that you are likely to feel better if you keep up with regular physical activity.
Exercise can boost your immune system, help relieve pain, stress, improve your mood, stimulate your appetite and help you sleep better. You should ask your healthcare provider about suitable forms of exercise, and find one you can enjoy.
Video: Tired of it – young women, metastatic breast cancer and fatigue
Fatigue is a common side effect of metastatic breast cancer treatment. Four young women living with metastatic breast cancer discuss how fatigue impacts their lives and their strategies for managing it.
The growth of some types of breast cancer is stimulated by the female hormone oestrogen and progesterone. In younger women who are still having periods, chemotherapy effectively shuts down the ovaries and stops them producing oestrogen. Stopping the body's oestrogen production, and blocking its action on the cancer, reduces the chances of the cancer coming back. However, this can create unwanted menopausal symptoms or cause an early menopause.
The older you are (and closer you are to natural menopause), the less likely it is that your ovarian function and fertility will go back to normal. For hormone-sensitive cancers, ongoing antihormonal drug treatment may also be recommended, which can also cause menopausal symptoms. Your healthcare provider and wider team will be able to give you advice on ways to reduce the impact of these symptoms.
Some types of treatment (eg, chemotherapy) can cause infertility, although this isn't the case for everyone and many women have their period return within a year after treatment. If having children is important to you, it may be possible to see a fertility specialist before your treatment starts, to look at your options for preserving your fertility. For many women, being unable to have children is a difficult reality to face. It's important to seek support from your partner, whānau, close friends, doctor and breast cancer team.
During treatment it's recommended that you use contraception, as you could still get pregnant over this time and the treatments can harm a developing pregnancy. It's usually advised that you use a reliable method of contraception for a couple of years after the end of treatment too. This is the time cancers are more likely to come back which may affect your decision about having a baby.
For women who become pregnant after finishing successful treatment, there's no evidence pregnancy increases the risk of breast cancer recurring.
About one in 20 breast cancers is caused by a faulty breast cancer (BRCA) gene. If yours was caused by such a gene, your healthcare provider can help you decide whether genetic testing would be helpful for your wider whānau.
It's natural to experience a sense of shock and sadness after breast cancer treatment.
Depending on the treatment you've had, your breasts may have scars, not match each other, or have a different texture or shape, which can be hard for some women to come to terms with. Your breast nurse is trained to help with any problems you may have, including scarring, skin rash and finding a suitable prosthetic breast to wear inside your bra. Your surgeon will be able to discuss breast reconstruction or implant options with you.
Time and having people to support can help you rebuild your confidence and regain your self-esteem. Image credit: Canva
Image credit: Canva
Breast cancer treatment can cause tiredness and stress, both of which can affect your sex drive (libido). The possible onset of menopause caused by treatment can also cause symptoms (eg, hot flushes, dry skin, vaginal dryness) that affect libido. If you're having menopausal symptoms, ask your healthcare provider about possible treatments and strategies to try.
Being intimate after breast surgery requires trust and may take time. At first, you may feel uncomfortable getting undressed in front of your partner. The best approach is to try to communicate how you are feeling, and whether you have any pain or skin tightening. Your partner may also be going through a difficult time in supporting you through this, so it's important to check in with each other. Counselling may be helpful to overcome issues around confidence or intimacy.
Depression and anxiety are common in women diagnosed with breast cancer. While it's common, it's not something you should deal with alone. Reaching out to your friends and whānau for support, or talking to your healthcare provider, is really important
Regular exercise can help to improve your mood, and help improve your sleep. Good sleep also improves your mood and energy levels as well. If sleep is a problem for you, it's a good idea to talk to your healthcare provider to see what can be done to help. You may find the Te Kete Haerenga sleep resource useful.
The Breast Cancer Foundation(external link) has a free phone service (0800 226 8773, 0800 BC NURSE) where a nurse can help with your questions and concerns.
The Breast Cancer Aotearoa Coalition(external link) has a list of counsellors you can reach out to.
33 tips on creating a great future after breast cancer
Baring it All(external link) is an eBook that gives practical tips to assist in rebuilding your life after cancer and guide you gently towards a life that you love.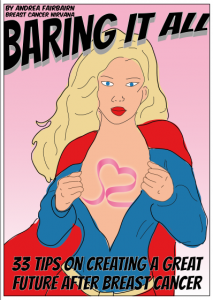
Image credit: Breast Cancer Nirvana
About the author
Andrea Fairbairn is a Pacific Island New Zealand woman who’s had breast cancer twice. She was diagnosed with breast cancer in 2007 and again in 2011. From her breast cancer experiences, she wanted to share her vision of making breast cancer easier and a positive life changing moment, rather than all nausea and hair loss.
Apps
Women's health apps
Mental health and wellbeing apps
Excerpts from Baring it all(external link)
- On a daily basis, think about how you would like to spend the day and do at least one thing just for you. Be kind to yourself.
- Get your health foundations right; if you need to, commit to eating a bit better and exercising today. Seek support from friends and family to improve your health.
- Rest when you are tired and stop before you over-exert yourself. Plan rest breaks each day and don't rush back into the work place at a million miles an hour.
- Acknowledge and celebrate what you have gone through and that you are a strong remarkable woman.
- Focus on your recovery and a positive future, not on the past or the unanswerable whys of cancer.
- Daily in a journal, write 3 things that you are grateful for.
References
- Breast cancer treatment options(external link) Breast Cancer Foundation, NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Phoebe Hunt, Sexual Health Registrar, Northland
Last reviewed:
Page last updated:





