If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Blood transfusion
Key points about blood transfusions
- A blood transfusion is a procedure where you receive blood or blood products from someone else through one of your veins.
- You might need a blood transfusion if you’ve lost a lot of blood, if your body isn't producing enough red blood cells or if chemotherapy is destroying your red blood cells.
- In Aotearoa New Zealand, blood used for transfusion only comes from unpaid or voluntary donors in New Zealand.
- Like any other procedure, a blood transfusion has its risks and complications, but it's generally safe and can save many lives.

What is a blood transfusion?
A blood transfusion is a procedure in which you're given blood or blood products through one of your veins. The procedure has to be done in hospital or at a healthcare facility.
Where does blood for a transfusion come from?
In Aotearoa New Zealand, blood for transfusion comes from unpaid and voluntary donors. Read about donating blood in New Zealand(external link).
Your healthcare provider will advise how much blood is needed in your situation. Many people get better after receiving just 1 unit of blood.
Blood transfusions are safe and can be lifesaving. Many surgeries or treatments for cancer can’t be done without blood transfusions.
You might need a blood transfusion because you don't have enough blood or red blood cells. Red blood cells are needed to carry oxygen around your body to help it function properly.
The image below shows the components of normal blood and their percentages.
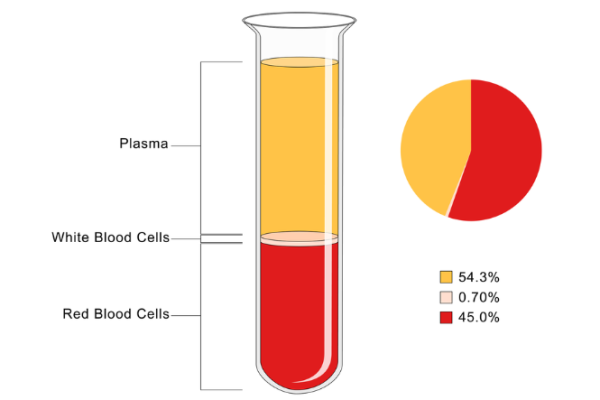
Image credit: Depositphotos
You might need a blood transfusion if:
- you've lost a lot of blood in an emergency situation, eg, in an accident or during surgery
- you've lost too much blood for other reasons, eg, heavy bleeding during a menstrual period or you have a stomach ulcer causing bleeding inside your body
- your body isn't producing enough red blood cells to carry oxygen around your body, eg, due to chemotherapy for cancer
- too many red blood cells are being destroyed in your body, eg, with haemolytic anaemia.
If you’re having elective (planned) surgery, you can reduce the chance of needing a blood transfusion during or after the operation by treating any iron deficiency or anaemia before your surgery. Talk to your healthcare provider about whether should get tested and treated for these. You should also discuss whether you need to stop taking certain medicines, such as warfarin and aspirin, that might increase your risk of bleeding and your need for blood transfusion during surgery.
A blood transfusion is an extremely safe procedure and can be lifesaving. Not having a blood transfusion when it's needed may lead to serious health problems.
The equipment used to collect blood is sterile and is only used once.
Before donor blood is given to you, it's always tested and screened for infections such as HIV/AIDS, hepatitis B, hepatitis C and syphilis. Both your blood and the donor blood are also tested to check for blood group types and antibodies to make sure they're compatible so that you don't have a bad reaction to the transfusion.
Your healthcare provider will consider the benefits and risks of a blood transfusion. If a blood transfusion is recommended it will mean the benefits are greater than the risks. Read more about the risks below.
Blood components that can be given in a blood transfusion include:
- Red blood cells – to replace your red blood cells if you have anaemia or severe bleeding.
- Platelets – to prevent or stop bleeding.
- Fresh frozen plasma and cryoprecipitate – to replace proteins for blood clotting, to prevent or stop bleeding.
Your doctor or nurse will explain the process of a blood transfusion, including the risks and side effects. You’ll need to sign a consent form if you agree to receive a blood transfusion. This is a good time to ask your healthcare providers any questions relating to the process. A sample of your blood will also be taken and tested for blood group types and antibodies. It will be matched with donor blood to prevent a reaction occurring between your blood and the donor blood.
Before any blood is given to you, a nurse will check your identification details to make sure you’re given the correct blood. Similar to a blood test, you’ll feel a prick or sharp sting when a needle is inserted into your vein, and some pressure when the blood is flowing into your vein. However, you shouldn’t feel any pain or discomfort during the process. A nurse will monitor you to make sure you feel fine during the transfusion.
A blood transfusion can take 1 to 4 hours per unit of blood being transfused.

Image credit: Depositphotos
Are extra units of blood helpful?
Your doctor will advise on how much blood you need. Many people get better after receiving 1 bag of donor blood. However some people will need more.
You may need more blood if you have:
- severe bleeding that's hard to control
- severe anaemia.
Blood transfusion in Aotearoa New Zealand is generally safe, however the risks increase if you get more blood. Research has found that extra units of blood aren't helpful if you don't need them.
There are other alternatives to a blood transfusion. These include the following:
- No transfusion – you may consider not having a transfusion, however, this isn’t recommended. If your doctor has decided that you need a transfusion as the risks from not having one are much greater than the risks from having a transfusion.
- Providing blood for yourself – this is called autologous blood collection and is where your own blood is collected for your use. In Aotearoa New Zealand, this is only done in special circumstances, such as if you have a rare blood type.
- Directed donations – this is where blood is collected from your relatives or friends. This is no safer than receiving blood from healthy donors so it's not done in Aotearoa New Zealand.
- Medicines and other techniques – there are medicines that can reduce blood loss or stop blood clots from being dissolved. There are also anaesthetic and surgical techniques that aim to reduce blood loss during surgery.
Talk to your doctor to find out what alternative is best for you.
It's important to note that alternatives to donor blood transfusion may not always be suitable in emergencies, eg, because of the planning needed ahead of time or the amount of blood loss you’ve experienced.
The risks of a blood transfusion include:
- temporary reactions such as a mild fever or skin rash. These occur in about 1% of people.
Other much rarer reactions include:
- Fluid overload because your heart can't cope with the volume of blood or the speed at which it's being given.
- An incompatibility reaction between you and the donor blood. This can lead to kidney failure, breathing problems and other life-threatening complications.
- A more severe allergic reaction such as fainting breathing difficulties or cardiac arrest.
- Minor virus infections, but this happens only occasionally.
- More serious infections such as hepatitis B, hepatitis C and HIV/AIDS. These are very rare as screening for these infections is done before the procedure.
- The blood transfusion not working as desired.
Seek immediate medical attention from the nearest emergency department or call 111 if you or someone you care for has the following symptoms during or after the procedure:
Some reactions can occur days after a blood transfusion. Ring Healthline 0800 611 116 for advice if you're not sure what to do. |
A general guide to blood transfusion – information for patients and families(external link) Health Translations Victoria, Australia
Blood transfusion(external link) NHS, UK
Brochures
Fresh blood components – your guide to blood transfusion(external link) NZ Blood Service Also available in te reo Māori(external link), Samoan(external link), French(external link), Korean(external link), Chinese(external link)
My guide to blood transfusion(external link) National Blood Authority & NPS MedicineWise, Australia
Receiving a blood transfusion – information for patients and their families, carers and guardians(external link) NHS, UK, 2021
References
- Fresh blood components – your guide to blood transfusion(external link) NZ Blood Service
- Receiving a blood transfusion – information for patients and their families, carers and guardians(external link) NHS, UK, 2021
- Transfusion medicine handbook – clinical alternatives and applications(external link) NZ Blood Service, NZ
Brochures
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: New Zealand Blood Service
Last reviewed: