- Bladder training is a main treatment. This can work well in up to half of cases.
- Pelvic floor exercises may also be advised in some cases.
- Medication may be advised instead of, or in addition to, bladder training.
- Surgery is sometimes recommended if the above methods have been unsuccessful.
Bladder training
The aim of bladder training is to slowly stretch the bladder so that it can hold larger and larger volumes of urine. In time, the bladder muscle should become less overactive and you should become more in control of your bladder. This means that more time can elapse between feeling the desire to pass urine, and having to get to a toilet. Leaks of urine are then less likely.
Bladder retraining is best undertaken with the guidance of a continence advisor or a practice nurse. The technique is to stay still and hold on until the feeling of urgency has passed, and then move to the toilet. Once you can do this, the aim is to lengthen the time between the urge passing and moving to the toilet. This technique requires persistence by you and support from your advisor or nurse.
You may find the urge to urinate happens at predictable times, such as on getting home or at the sound of running water. Recognising your triggers and not going to the toilet when triggers create the urge helps break the association and is another part of bladder retraining.
Helpful lifestyle changes include avoiding bladder irritants such as caffeine, alcohol and carbonated drinks, at least while you are attempting bladder retraining.
Pelvic floor exercises
Regular exercises to strengthen your pelvic floor muscles can help you to avoid leaking urine when your bladder muscles contract at unpredictable times. These should be learned at the same time as bladder retraining, with help from a continence advisor if needed.
See: Pelvic floor training for women and men
Medicines for overactive bladder
There are several medicines, called anticholinergics, that act on the bladder muscles to help reduce the frequency and severity of contractions. They can provide some immediate benefit and help you control your bladder while you learn the exercises and techniques described above. After a time, when you have regained bladder control, it may be possible to slowly reduce and stop using the medicines. A dry mouth or indigestion are possible side effects with these drugs.
Women can experience oestrogen hormone deficiency, which has been associated with urinary urgency and frequency. Vaginal oestrogen cream has been shown to reduce these symptoms.
The ‘simple’ combined approach described so far is known to be effective for about half of people with urge incontinence. If there has been no improvement despite guidance from a continence advisor, your doctor may refer you to a specialist, called a urologist, who can investigate the problem further and consider other treatments. One of these is botulinum toxin injections at sites within the bladder, a procedure that does not normally require a hospital stay and may provide relief for up to a year.
Surgery
If the above treatments are not successful, surgery is sometimes suggested to treat overactive bladder syndrome. Procedures that may be used include:
Sacral nerve stimulation
An overactive bladder can be treated by sacral nerve stimulation. A small pulse generator device is implanted under the skin of the buttock to send a burst of electrical signals to the nerves that control the bladder.
Augmentation cystoplasty
In this operation, a small piece of tissue from the intestine is added to the wall of the bladder to increase the size of the bladder. However, not all people can pass urine normally after this operation. You may need to insert a catheter (a small tube) into your bladder in order to empty it.
Urinary diversion
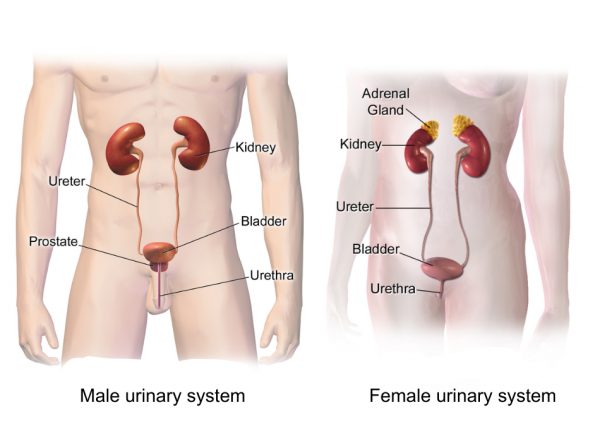
In this operation, the ureters (the tubes from the kidneys to the bladder) are routed directly to the outside of your body. There are various ways that this may be done. Urine does not flow into the bladder. This procedure is only done if all other options have failed to treat your overactive bladder syndrome.