If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Benign paroxysmal positional vertigo (BPPV)
Key points about benign paroxysmal positional vertigo (BPPV)
- Benign paroxysmal positional vertigo (BPPV) is an inner ear disorder that can lead to sudden vertigo – a type of dizziness that feels like a spinning sensation.
- Vertigo in BPPV tends to last for less than a minute and is brought on by head movements such as rolling over in bed or looking upwards.
- It’s caused by calcium crystals (otoconia) in the fluid in your ear moving to a place in your ear where they shouldn’t be.
- BPPV is more common in people over the age of 40 and it often gets better on its own within weeks to months.
- Treatment of BPPV includes doing specific movements designed to shift the crystals in your inner ear back to where they should be.

Benign paroxysmal positional vertigo (BPPV) is a condition that affects your inner ear and can lead to sudden episodes of vertigo. Vertigo is a type of dizziness where you feel like you or your surroundings are spinning.
BPPV is a common cause of vertigo and is more common for older people. It usually causes short episodes of intense vertigo when you move your head in certain directions, such as when you roll from one side to the other in bed. It’s caused by the movement of tiny crystals in your inner ear that have become loose.
BPPV usually gets better on its own after a few weeks to months and there are exercises you can do to help ease the symptoms.
Having BPPV can increase your risk of falls because the vertigo can make you feel unsteady and lose your balance.
Your ears are made up of 3 parts – the outer ear, the middle ear and the inner ear. Benign paroxysmal positional vertigo (BPPV) is a condition that affects your inner ear.
The diagram below shows the structure of your inner ear. It includes the cochlea, utricle and semicircular canals (called ducts in the image below). The cochlea helps with hearing, while the utricle and the semicircular canals help with balance and posture.
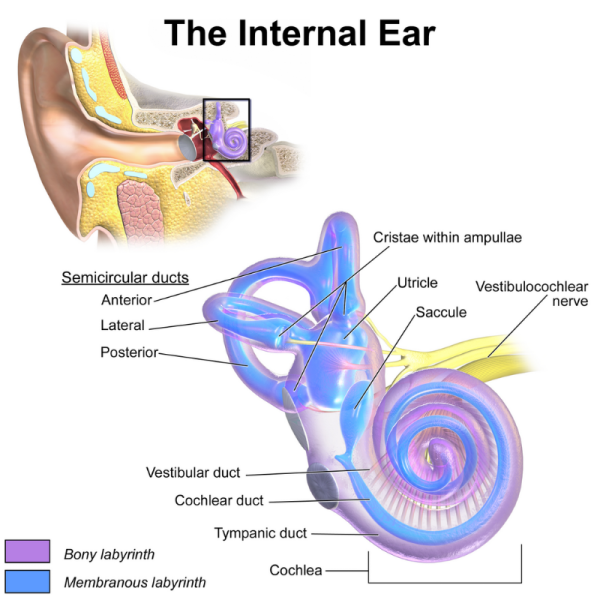
Image credit: Blausen via Wikimedia Commons(external link)
The fluid in the utricle contains calcium crystals called otoconia. These crystals can move out of the utricle and into one of the semicircular canals where they disrupt the usual way your brain interprets head movement. Your brain gets confused between these abnormal signals and the normal signals from your other ear, resulting in vertigo.
It's not clear why some people have these loose calcium crystals, but it’s thought to be related to increasing age – BPPV is more common in people over the age of 40. You’re also at higher risk of BPPV if you’re a woman, if you had a previous head or ear injury, or infection in your inner ear. Having low levels of vitamin D or osteoporosis (low bone density) may make the calcium crystals more likely to break loose.
The main symptom of BPPV is vertigo which is a type of dizziness where you feel that you or your surroundings are moving or spinning when there’s no actual movement.
In BPPV, the vertigo is triggered by sudden changes in the position of your head, such as when you tip your head up or down, lie down, or turn over or sit up in bed. It tends to last for a minute or less and settles if you keep your head still.
You may feel light-headed or unsteady and you may lose your balance. Some people feel as though they’re spinning around or falling. You may also feel nauseous (sick) but vomiting (being sick) is rare.
Usually, symptoms get better within a few weeks or months, but for some people they continue to come and go over months to years.
You should see a healthcare provider if:
- your vertigo doesn’t go away or keeps coming back
- you also develop hearing loss or tinnitus (ringing in your ear)
- your symptoms are having an impact on your daily life.
- facial drooping, trouble speaking or swallowing
- leg or arm weakness, numbness or tingling
- difficulty walking, falling over, poor coordination or confusion
- a severe headache or neck pain
- vomiting (being sick) or feeling very sick
- a very high temperature or feeling hot and shivery
- double vision or loss of vision
- hearing loss that gets worse, especially on one side.
Vertigo could be a sign of a more serious medical condition such as a stroke, circulation problems or an infection. If you’re not sure what to do call Healthline free on 0800 611 116 for health advice and information anytime.
Your healthcare provider will ask you about your symptoms, including whether they’re related to any particular head movements. They’ll also find out whether you have other symptoms such as hearing loss or fullness in your ear to rule out any other diagnosis.
No blood test is needed to diagnose BPPV, but your healthcare provider may order some blood tests or further tests to rule out other conditions. They’ll also examine your ears and eyes and check your balance and how your nerves are working.
The main test to help diagnose BPPV is called the Dix-Hallpike test. For this test, an experienced healthcare provider moves your head and body in particular ways and looks for certain eye movements (known as nystagmus) that are seen in people with BPPV. The test doesn’t hurt, but it may bring on an attack of vertigo and possibly nausea and vomiting.
Video: Dix-Halpike manoeuvre for vertigo
This video shows the movements involved in the Dix-Hallpike test to diagnose BPPV.
Symptoms of BPPV often clear up within a few weeks or months without treatment. However, if your BPPV is ongoing or your symptoms are affecting your daily life, treatments include:
- the Epley Manoeuvre
- Brandt-Daroff exercises.
Your healthcare provider or physiotherapist can tell you if these exercises are suitable for you. The exercises can bring on symptoms of BPPV, but these should gradually go away.
The Epley Manoeuvre is a procedure that your healthcare provider can perform on you and then teach you how to do yourself at home if it's appropriate. This exercise aims to shift the loose calcium crystals in your inner ear away from where they’re causing problems. The process is similar to the Dix-Hallpike test described above with a few extra movements. After the Epley is done your healthcare provider may suggest simple precautions with sleep and activity in the next several days to reduce the chances of the crystals shifting and causing problems again.
The video below explains how the Epley Manoeuvre is done.
Video: Epley Maneuver – performed on a patient suffering from vertigo
Brandt-Daroff exercises
The Epley manoeuvre may not be suitable if you have back or neck problems. Your healthcare provider may recommend Brandt-Daroff exercises. You need to do these 2 to 3 times a day for about 2 to 6 weeks. These exercises involve turning your head and movement of your upper body.
Read more about Brandt-Daroff exercises(external link) or watch the video below about how to do the exercises.
Video: Vertigo treatment with Brandt-Daroff exercises
Ask your healthcare provider or physiotherapist about how to perform this exercise.
If your BPPV is affecting your daily life and doesn’t improve with the Epley manoeuvre or Brandt-Daroff exercises, your healthcare provider may refer you to an ear, nose and throat (ENT) specialist.
Apps reviewed by Healthify
You may find it useful to look at some vertigo apps.
To help with the symptoms of BPPV:
- get out of bed slowly – sit on the edge of the bed for a bit before standing up
- avoid doing things where you have to move your head to look up, such as painting walls or ceilings, or looking for something up high
- sit down when you feel dizzy
- do the special exercises for BPPV (Epley manoeuvre or Brandt-Daroff exercises) if recommended by your healthcare provider.
If you have BPPV, you’re at risk of falls or accidents because episodes of vertigo can affect your balance and may make you feel unsteady.
To reduce your risk of a fall or accident:
- get out of your bed or chair slowly
- wear low-heeled shoes that fit properly
- use handrails on stairs.
For problematic or persistent vertigo:
- consider putting grab bars in your bathroom – don't use towel racks for balance
- use a shower stool
- put adhesive strips on the base of your shower or bath
- use a walking aid if needed.
For work health and safety:
- let your employer know about your symptoms, especially if your job involves operating machinery or climbing ladders
- avoid driving if you have vertigo symptoms (read more about driving and BPPV below).
Apps reviewed by Healthify
You may find it useful to look at some falls prevention apps.
If you have vertigo, it can be extremely dangerous to drive. It's important to let your healthcare provider know so they can treat your BPPV accordingly.
It’s also a legal requirement for you to drive only when you're medically fit, which means you shouldn’t drive if you’re dizzy or experiencing vertigo. You’ll need to stop driving until your condition has been treated and you have no more attacks of vertigo.
BPPV usually goes away by itself after a few weeks or months and many people never need treatment. However, if it keeps happening you should see a healthcare provider, especially if you’re older and a little unsteady as there’s a risk of falls if you have BPPV.
For some people, BPPV returns months or years later, and sometimes the symptoms go on for years. For the most part, however, BPPV is treatable with exercises such as the Epley manoeuvre or Brandt-Daroff exercises.
The following links provide further information about BPPV. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Benign paroxysmal positional vertigo (BPPV)(external link) The NZ Society for Balance, Dizziness and Vertigo, NZ
Benign paroxysmal positional vertigo(external link) Patient Info, UK
Benign paroxysmal positional vertigo (BPPV)(external link) The Vestibular Disorders Association (VeDA), US
Benign paroxysmal positional vertigo (BPPV)(external link) Better Health Channel, Australia
Vertigo(external link) NHS, UK
Brochures
Benign paroxysmal positional vertigo – patient information(external link) BMJ Best Practice, UK, 2022
Brandt-Daroff exercises to treat BPPV(external link) University Hospital Southampton NHS Foundation Trust, UK, 2024
Vertigo (BPPV)(external link) Safer Care Victoria, Australia, 2019
Apps
Vertigo apps
Falls prevention apps
References
- Benign paroxysmal positional vertigo(external link) Patient Info, UK, 2025
- Benign paroxysmal positional vertigo (BPPV)(external link) The Vestibular Disorders Association (VeDA), US
- Vertigo(external link) Auckland Regional HealthPathways, NZ, 2022
- A delicate balance – managing vertigo in general practice(external link) BPAC, NZ, 2012
- An approach to vertigo in general practice(external link) Australian Family Physician, 2016
- Cole SR, Honaker JA. Benign paroxysmal positional vertigo – effective diagnosis and treatment(external link) Cleve Clin J Med. 2022; 89(11):653–662
- Koshi EJ, Sutton AE. Benign paroxysmal positional vertigo(external link) StatPearls, NIH, US, updated 2025
What are the symptoms of BPPV?
The main symptom of BPPV is vertigo – which is a feeling that you or your surroundings are moving or spinning when there’s no actual movement. If you have BPPV, vertigo usually lasts less than a minute. It’s triggered by head movements (eg, when you get out of bed or roll over in bed), and stops if you keep your head still. You may also have nausea (feel sick) or feel unsteady or light-headed.
What is the treatment for BPPV?
BPPV often goes away after several weeks or months, without any treatment. However, there are exercises that can help your symptoms. These involve moving your head in particular ways to shift the calcium crystals in your inner ear that are causing the symptoms. You may be able to do the exercises by yourself, (but having someone with you in case you lose your balance is a good idea) or you may need assistance from somebody trained in administering the exercises, such as a physiotherapist.
How long does BPPV last?
An episode of BPPV lasts about 20 to 30 seconds and usually less than a minute. Most people find their symptoms get better within weeks or months, but episodes can come and go and sometimes symptoms can go on for years. See a healthcare provider if your symptoms are bothering you or don’t go away.
Brochures

Vertigo (BPPV)
Safer Care Victoria, Australia, 2019

Brandt-Daroff exercises to treat BPPV
University Hospital Southampton NHS Foundation Trust, UK, 2024
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Grace Lee, FRNZCGP and Clinical Educator
Last reviewed:





