Basal thumb arthritis
Also known as carpometacarpal joint osteoarthritis
Key points about basal thumb arthritis
- Osteoarthritis is the most common form of arthritis to affect the joint at the base of your thumb.
- The basal thumb joint allows a great range of movement which makes it more likely for problems to develop over time.
- You're at greater risk if you are female, over 40 years old, have had a previous injury to the area or your job involves repetitive movement of your thumb.
- Common symptoms include pain, swelling, stiffness, loss of grip and fine control, and muscle weakness of your thumb.
- There's no cure, but treatment and self-care aim to ease your symptoms, prevent the joint from getting worse and reduce the impact osteoarthritis has on your daily life.

The joint at the base of your thumb is known as the basal joint. It is where the carpal bone (trapezium) meets the first metacarpal bone of your thumb. The joint is also known as a carpometacarpal (CMC) joint.
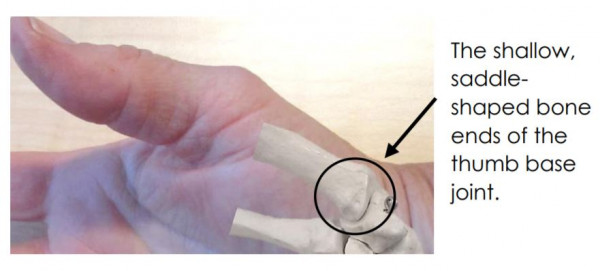
Image credit: Miranda Buhler
The thumb base joint is a small joint that gets put under a lot of force with every-day use. The ends of the 2 bones are a shallow saddle-shape and sit together like a rider on a saddle. This allows a lot of movement but is not very stable.
If the short ropes that hold the bones together (ligaments) and muscles are not keeping the bone ends well-aligned or under a lot of stress and strain, then the force that goes through the joint can cause injury to the covering on the bone ends (cartilage), ligaments and bone.
This gradual injury can cause swelling (inflammation), reduce movement and result in pain in the base of your thumb. Recovery may be limited by repeated stress and strain and other factors such as age.
The basal joint is a very mobile joint, which allows the wide range of movement we need for hand use such as grip, pinch, and fine manipulation. This high mobility leaves the joint with poor stability, which increases the risk of damage to the tissues around the joint.
You are more at risk if:
- you are more than 40 years old
- your work involves repetitive movement or loading of your thumb
- you have had a previous injury or fracture to your basal thumb
- you have other family members with thumb base osteoarthritis.
Symptoms of basal thumb arthritis include:
- pain at the base of your thumb that worsens during activity
- pain at the base of your thumb that bothers you during the night
- loss of grip strength and fine control
- stiffness that is worse in the morning
- swelling at the base of your thumb
- a bony bulge at the base of your thumb
- creaking or cracking sensations with thumb or hand movement
- deformed thumb joints if the condition progresses to a later stage.
Your doctor will ask what you are able to do and what makes your pain worse. A physical examination will be carried out with close attention to your basal thumb joint. There are no specific blood tests for basal thumb arthritis, but tests may be made to exclude other forms of arthritis such as rheumatoid arthritis and septic arthritis.
X-rays are not needed to diagnose basal thumb arthritis but can be helpful in some instances. X-ray findings are not a good guide to how severe symptoms may become and x-ray findings do not match the amount of pain or impairment you experience. X-rays are usually only helpful if it has been decided that you need surgery, to help the surgeon plan what surgery they should do.
Treatment for osteoarthritis cannot cure the condition, but can help with:
- reducing the pain
- maintaining your ability to work or do activities you enjoy
- reducing how often your joint becomes inflamed and painful (flare-ups)
- preventing joint changes from getting worse.
Your doctor, physiotherapist, hand therapist or occupational therapist is likely to recommend treatment that takes into account the severity of the condition, your symptoms, other medical conditions, your age, job and everyday activities.
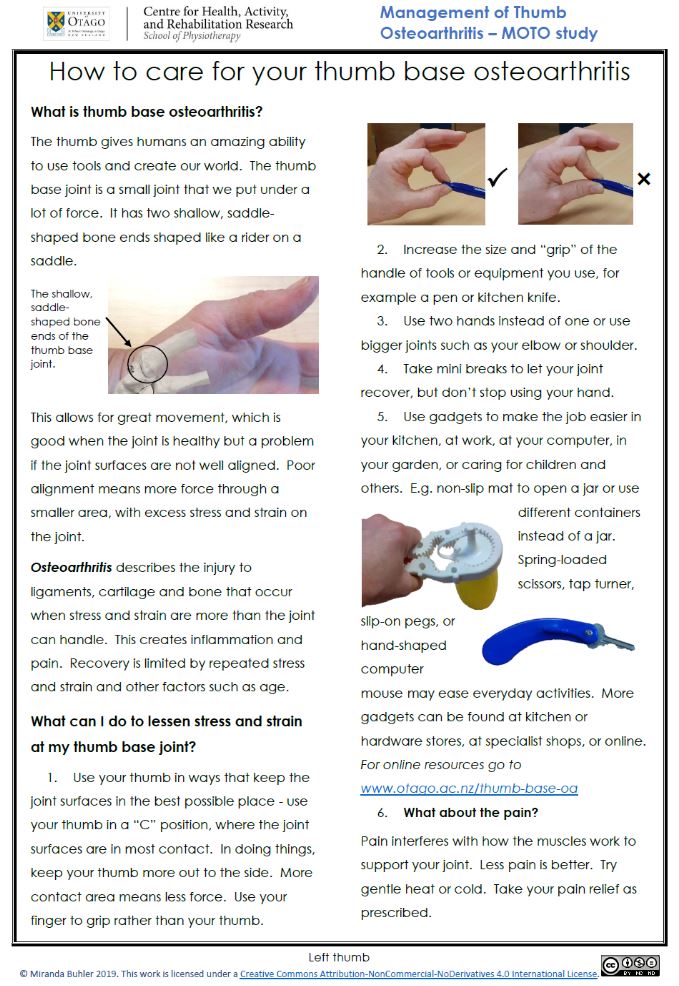
Changes to your lifestyle
How you manage day-to-day activities can make a big difference in the impact basal thumb arthritis has on your lifestyle. Self-care measures that may be helpful include:
- using your thumb in a position where the joint surfaces are in most contact, eg, your thumb and index finger should make a circle when holding objects, not collapsing towards each other
- taking frequent breaks when doing activities that involve your thumb
- using bigger joints such as your shoulder or elbow joint to carry out daily activities
- using 2 hands instead of one hand
- using special equipment to ease activities such as opening jars
- modifying equipment that is skinny or difficult to hold by making it fatter, and easier to grip
- wearing a splint to support you thumb
- applying cold packs or gentle heat to reduce swelling and relieve pain – a good pair of warm gloves will help in winter
- 'arthritis gloves' can help to keep your hand and thumb warm and give light compression, which may help with swelling and pain.
Hand exercises
Doing suitable hand exercises can make a difference. These are hand exercises you can try now for left basal thumb osteoarthritis [PDF, 333 KB] and right basal thumb osteoarthritis [PDF, 333 KB]. A physiotherapist or hand therapist can provide more information about hand exercises.
Medication
Medication for basal thumb arthritis focuses mainly on pain relief. Usually, the approach is to try the milder pain relief medications first, such as paracetamol and non-steroidal anti-inflammatory (NSAIDs) gels or sprays.
If that does not provide relief, your doctor will advise you to move to the stronger pain relief medications, such as oral NSAIDS, or steroid injections in some cases. This approach reduces the risk of side effects. The gel NSAIDs have been shown to be more effective than the oral NSAIDs for basal thumb arthritis.
- Paracetamol is recommended as the pain reliever to try first. It is best taken regularly and not just when you have pain.
- Gels or sprays (also called topical agents) are useful for people with mild-to-moderate pain. Examples include NSAID gels or sprays such as ibuprofen gel, diclofenac gel or Voltaren gel and capsaicin cream.
- Oral (NSAIDs) have not been shown to be helpful in basal thumb arthritis.
- Steroid injections are given into the painful joint to reduce inflammation. These are reserved for extremely painful osteoarthritis and used for treating flares.
Read more about medications on the osteoarthritis page.
Surgery
If joint changes, pain and disability are all severe and a comprehensive management programme including the above measures is not helping, surgical procedures such as removing the trapezium, carpal and metacarpal bone fusion or joint replacement may be necessary. Your GP may be able to provide more details about different surgical options.
Apps reviewed by Healthify
You may find it useful to look at some arthritis apps.
Related topics
The following links have more information about osteoarthritis. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Arthritis of the thumb(external link) HealthInfo Canterbury, NZ
Osteoarthritis(external link) Arthritis New Zealand
Osteoarthritis of the carpometacarpal thumb joint(external link) NHS, UK
Arthritis of the thumb(external link)(external link) OrthoInfo, US
Apps
Resources
How to care for your thumb Miranda Buhler, 2019 Right thumb [PDF, 333 KB] Left thumb [PDF, 333 KB]
References
- First carpometacarpal joint osteoarthritis(external link) Auckland Regional HealthPathways, NZ
- Arthritis of the thumb(external link) HealthInfo Canterbury, NZ
- Arthritis of the thumb(external link) OrthoInfo, US
Continuing professional development
Hand therapy – Craig Hawkyard(external link) (Craig Hawkyard, NZ, 2016)
Wrist and hand conditions – Tom Sharpe(external link) (Tom Sharpe, NZ, 2016)
Clinical resources and publications
- Buhler M, Chapple CM, Stebbings S, Potiki-Bryant KA, Baxter GD. Impact of thumb base osteoarthritis – a pragmatic qualitative study(external link) Arthritis Care and Research. 2019. Advanced online publication. https://doi.org/10.1002/acr.24124
- Buhler M, Chapple CM, Stebbings S, Sangelaji B, Baxter GD. Effectiveness of splinting for pain and function in people with thumb carpometacarpal osteoarthritis: a systematic review with meta-analysis(external link) Osteoarthritis and Cartilage. 2019;27:547-559. https://doi.org/10.1016/j.joca.2018.09.012
- Buhler M, Chapple CM, Stebbings S, Adams J, Gwynne-Jones D, Baxter GD. Splinting for thumb carpometacarpal osteoarthritis: protocol for a feasibility randomized controlled trial(external link) Physical Therapy Reviews. 2020. https://doi.org/10.1080/10833196.2020.1763662
Apps
Brochures
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Miranda Buhler, physiotherapist and hand therapist
Last reviewed:
Page last updated:






