Appendicitis
Key points about appendicitis
- Appendicitis is the inflammation of your appendix – a small, finger-like pouch in your gut wall.
- It's unclear why an appendix becomes inflamed but it may be due to a blockage caused by poo or undigested food.
- The main symptom is tummy pain that starts around your belly button and moves to your lower right tummy as it gets worse.
- Appendicitis can cause complications such as infection and inflammation, which can be life threatening.
- Get medical help quickly if you have the symptoms below.
- Treatment usually involves surgery to remove your appendix.

| Call 111 or go to the nearest emergency department immediately if you or someone you care for experiences the following: |
|
Appendicitis usually affects young people aged 10–20 years but can happen at any age.
Your appendix is a small, closed-end tube around 5–10 cm long located at the beginning of your large bowel (colon). It is situated in your right lower tummy area. The function of the appendix is not known, but it is safe to live without it.
It's also not clear why an appendix becomes inflamed. It may be due to a blockage caused by a faecal matter (poo) or undigested food. This provides a rich breeding ground for bacteria, causing your appendix to become infected, swollen and full of pus.
The blockage could also be caused by a tumour in older adults or a swollen lymph node in your gut due to an upper respiratory tract infection.
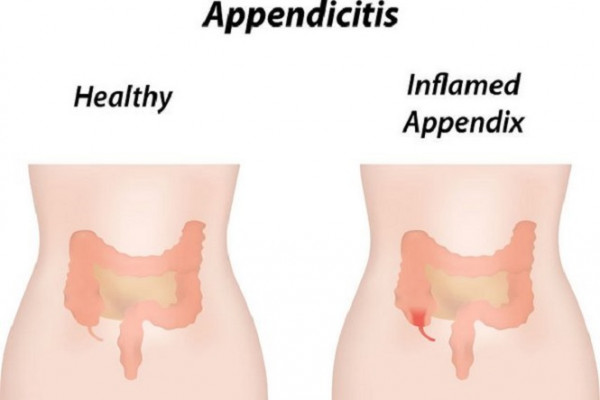
Image credit: 123rf
The main symptom of appendicitis is tummy pain. At first, you may notice a dull pain around your naval (tummy button). As the inflammation gets worse, the pain becomes sharper and may move down to the lower right-hand side of your tummy.
The pain rapidly worsens and over 6–24 hours can become more severe. If you gently press this area of your tummy it can make the pain worse. Coughing or walking may also worsen the pain.
Not all cases of appendicitis follow this ‘classic’ course. In some cases, the pain is felt higher in your tummy, particularly if you are pregnant, or closer to your anus (back passage). In other cases the pain is quite mild and does not become severe until the appendix bursts.
Other symptoms may include:
- fever
- nausea (feeling sick)
- vomiting (being sick)
- diarrhoea (runny poos)
- constipation (hard poos)
- loss of appetite.
If you have any of the symptoms above, contact your GP urgently.
Appendicitis can cause complications, including:
- peritonitis
- abscess.
Peritonitis
If you have appendicitis and don’t seek medical treatment, the inflammation can get worse and your appendix can burst. Once your appendix bursts, the entire lining of your abdomen (the peritoneum) can become infected with bacteria, and this can cause severe pain to your whole abdomen (tummy area). This is known as peritonitis (the inflammation of your peritoneum). Peritonitis is life threatening and needs to be treated immediately by antibiotics and surgery to remove your appendix.
Symptoms of peritonitis can include:
- severe continuous tummy pain
- your tummy feels hard and tight
- your tummy appears swollen
- fever (high temperature)
- nausea (feeling sick) and vomiting (being sick)
- fast heartbeat
- shortness of breath or rapid breathing
- coughing
- any movement, particularly of your legs at your hips, is painful.
Abscess
After your appendix bursts, pus can collect around it and form a lump or mass where your body is trying to fight off the infection. This can cause pain around your right lower tummy area. If this happens, you will need surgery to drain the pus, as well as to take antibiotic medicine.
Your GP or doctor will ask you questions related to your symptoms and examine you, pressing your right lower tummy to see if the pain gets worse. Your doctor may also order tests to confirm the diagnosis and rule out other conditions that can have the same symptoms.
Tests that may be done include:
- a blood test to look for infection
- a pregnancy test if there is a possibility you could be pregnant
- a urine (pee) test to rule out urine infection
- a CT scan.
If you are very unwell, you may be sent to the hospital immediately and have these tests in the hospital. The hospital may also do a CT scan to confirm the diagnosis.
Treatment is normally surgery (an operation) to remove the inflamed appendix before it bursts. If you are very unwell, your surgeon may operate straight away rather than ordering more tests. If you don’t need surgery urgently, you may be given antibiotics and observed for a time.
The surgery is called an appendicectomy or appendectomy. The procedure can be done through a keyhole surgery (laparoscopic) or an open surgery. Your surgeon will let you know the best treatment options for you and discuss the possible risks of each surgery.
Laparoscopic appendectomy
In straightforward, non-complicated situations, your surgeon will often perform the appendectomy using the keyhole technique. This involves making very small cuts or holes in your tummy and inserting a video camera and surgical tools to remove the appendix without the need for a larger cut. This technique is usually preferred as the recovery is quicker than an open surgery.
Open appendectomy
In some cases, an open approach is use, in which a slightly larger cut is made on your right lower tummy area to remove your appendix. This technique is usually used if:
- your appendix has burst and formed a lump or mass around it
- you have had an open abdominal surgery previously.
If your appendix has already ruptured and you have peritonitis, a larger cut in the middle of your tummy (laparotomy) may be needed to remove your appendix and wash out the fluid contents that have leaked from the ruptured appendix.
Once you have been discharged from hospital after your surgery, you need to:
- care for your incision (surgery) site
- drink plenty of fluids and eat more fibre
- attend follow-ups and see your doctor again
- limit your activity
- manage your pain.
Care for your incision (surgery) site
- Keep the site of the surgery clean and wash it daily with gentle soap and water.
- Your doctor will tell you when you can remove the dressing.
- This will normally be 48 hours after the surgery.
- You may have dissolvable stitches, or regular stitches that need to be removed at a later date.
- Ask your surgeon or doctor when you need to go back and get the stitches removed.
Read more about caring for your surgical wound at home.
Drink plenty of fluids and eat more fibre
- You may have constipation (hard poos) for a short period after your surgery.
- It will help if you eat plenty of fibre and drink plenty of fluids.
- It is also important not to take codeine painkillers as these can worsen your constipation.
- Your GP can prescribe you some medicine if your constipation is troublesome.
See your doctor again
- You will usually have a follow-up visit 10–14 days after your surgery.
- In the meantime, call your doctor immediately if any of the following signs of infection develop:
- fever
- new redness spreading outward from your incision site
- pus or other drainage from your incision
- sudden onset of severe nausea/vomiting
- new and worsening severe abdominal (tummy) pain.
Limit activity
- Do not do any heavy lifting or strenuous activity until you have been seen at your check-up appointment.
- Ask your surgeon about when is safe to return to your regular job.
- This will depend on the type of work you do and whether your appendectomy was laparoscopic or open (see treatment above).
Manage pain
- In most cases, pain felt after surgery should be minimal after the first few days.
- Your surgeon will provide you with a prescription for pain relief medicines.
- You can take the pain relief medicine if necessary.
Appendicitis(external link)(external link) HealthInfo Canterbury, NZ
Appendicitis – a patient’s guide(external link)(external link) Family Doctor, NZ
Appendicitis(external link)(external link) Patient Info, UK
Appendicitis(external link)(external link) NHS, UK
References
- Appendicitis, suspected(external link)(external link) Starship Clinical Guidelines, NZ, 2020
- Appendicitis(external link)(external link) Patient Info, UK
- Appendicitis(external link)(external link) KidsHealth, NZ
Clinical resources
Appendicitis, suspected(external link) Starship Clinical Guidelines, NZ, 2016
Telehealth clinical module – abdominal assessment(external link) ProCare, NZ, 2022
How to improve the clinical diagnosis of acute appendicitis in resource limited settings(external link) Alvarado World Journal of Emergency Surgery, 2016
Appendicitis(external link) MSD Manuals, US
Continuing professional development
Podcast
Appendicitis controversies(external link) Emergency Medicine Cases, Canada
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Sarah Hyder, Clinical and Quality Manager, Primary Options for Acute Care (POAC), Auckland
Last reviewed:
Page last updated:





