Delirium
Key points about delirium
- Delirium is a change in a person’s mental ability that results in confusion, problems paying attention and a lack of awareness of one’s surroundings. It usually starts suddenly and can come and go.
- It’s common in older people and people with many health problems.
- It usually has 1 or more underlying causes. Many people make a full recovery once these have been treated.
- Risk factors include being over 65 years of age, having dementia, a hip fracture or severe illness, and being an older person in hospital.

- infections – especially of the bladder or kidneys (called a urinary tract infection or UTI), chest or skin
- medicines – especially for pain, anxiety or sleep
- surgery or serious injury, including broken bones
- heavy alcohol use or withdrawal
- strokes
- diabetes that's not well controlled
- heart, kidney or liver failure
- dehydration, lack of sleep or constipation
- unrelieved pain or stress.
- not being aware of the correct time and place
- poor concentration, confusion, or trouble remembering recent things
- a disturbed sleep-wake cycle, including sleeping in the day and being awake at night
- hallucinations (seeing or hearing things that aren’t there) or delusions (false beliefs)
- being unusually upset, anxious, angry or suspicious without good reason
- being withdrawn and drowsy.
Diagnosis
Your healthcare provider will want to find out the underlying cause of your delirium, so will ask you, your friends or loved ones about your symptoms and your medical history. They will also do a physical examination and blood tests.
Treatment
If you have mild symptoms you will receive treatment at home for the underlying cause of the delirium. If you have severe delirium, you may be admitted to hospital and receive medicines.
Video: What are the consequences of having delirium?
This video may take a few moments to load.
(iDelirium, 2019)
The following may help you or someone you are caring for with delirium:
- reminders of the time or day, eg, clocks and calendars
- making sure to use hearing aids and glasses
- comfortable amounts of light, noise and heat or cold
- plenty of rest and moderate amounts of activity – don't overdo it!
- enough sleep, healthy food, water, movement and regular use of the toilet.

Image credit: Canva
The PINCHES ME Kindly(external link) approach can be useful to help avoid delirium in older people and sick people:
- Pain – manage with the help of your healthcare provider. Read more about pain.
- Infection – avoid by going to the toilet regularly, checking your skin for redness or irritated areas, telling your healthcare provider about any fevers (high temperatures).
- Nutrition – eat plenty of good food. Read more about healthy eating.
- Constipation – avoid by going to the toilet regularly, and talking to your healthcare provider if you're not opening your bowels (passing poo) as usual. Read more about constipation.
- Hydration – drink plenty of water.
- Exercise – do appropriate amounts of exercise but don't overdo it.
- Sleep – regular sleep is important. Talk to your healthcare provider if you're not sleeping well. Read some sleep tips.
- Medication – only as necessary. Talk to your healthcare provider occasionally to see if there are any medicines you no longer need. Read more about medicine reviews.
- Environment – calm and quiet is better that noisy or busy. Keep glasses and hearing aids nearby and use them when needed.
'Kindly' refers to the need to be supportive and compassionate.
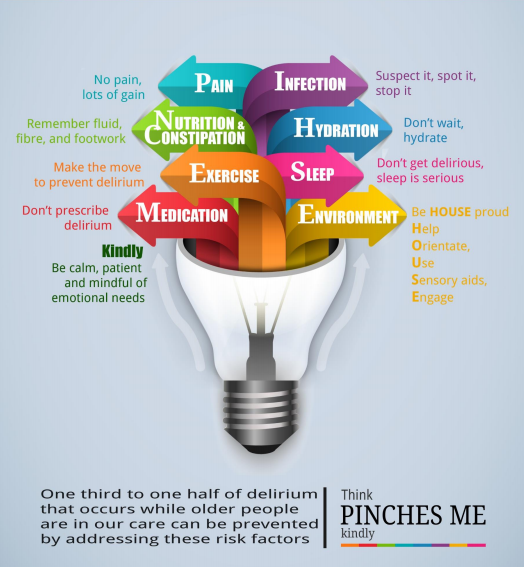
Image credit : Think Delirium prevention project – PINCHES ME kindly(external link) Canterbury District Health Board, NZ
Delirium in older adults(external link) Health in Ageing, US
Delirium (acute confusion) – information for patients, families and friends(external link) Carers NZ
Resources
Preventing delirium while in hospital [PDF, 836 KB] South Island Alliance, NZ
Ideas for older people to help prevent delirium [PDF, 669 KB] South Island Alliance, NZ, 2019
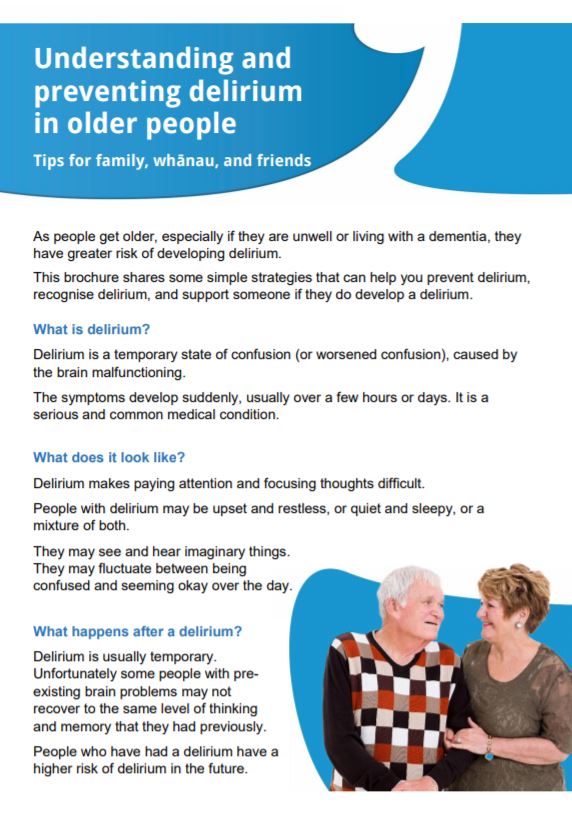
Understanding and preventing delirium in older people [PDF, 1.6 MB] South Island Alliance, 2019
THINKdelirium(external link)(external link) Canterbury District Health Board, 2016
Delirium information for patients(external link)(external link) Waitematā DHB, NZ, 2019
Prevention, detection, assessment & management of delirium(external link)(external link) Waikato DHB, NZ
References
- Holden J, Jayathissa S, Young G. Delirium among elderly general medical patients in a NZ hospital(external link) Internal Medicine Journal 2008;38(8):629-634.
- Young J, Inouye SK. Delirium in older people(external link) BMJ (Clinical research ed.) 2007;334(7598):842-846.
- What’s delirium and how does it happen?(external link) Healthline, US, 2022
- (external link)Delirium and acute confusional states – prevention, treatment, and prognosis(external link) UpToDate, US, 2023 (login needed)
Consultation
Delirium is easily misdiagnosed, so don’t assume confusion is due to long-term dementia or intellectual handicap even in the elderly and those with learning difficulties. It’s important to do a differential diagnosis between delirium, dementia and depression
- Confirm diagnosis using 4AT assessment test for delirium and cognitive impairment(external link) 4AT.com
- For further information for health practitioners, see Delirium(external link) on patient.info.
Clinical resources
Delirium – te mate kuawa(external link) Frailty care guides Health Quality & Safety Commission, NZ, 2023
Delirium aware – a toolkit to facilitate quality improvement for hospital teams working with older people South Island Alliance, NZ, 2019
Delirium aware – a toolkit to facilitate quality improvement for aged residential care facilities South Island Alliance, NZ, 2019
Delirium balloon analogy – why is delirium more common in older people Delirium Care Network
Kids get delirium too – what to know about delirium in kids Delirium Care Network
Delirium guide for healthcare administrators Delirium Care Network
Managing delirium and psychological symptoms in the last days of life(external link) BPAC, NZ, 2023
Brochures
South Island Alliance, 2019
South Island Alliance, NZ, 2019
South Island Alliance, NZ, 2019
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator.
Last reviewed:





