Clinical pathways and guidelines
Constipation(external link) Starship Clinical Guidelines, NZ, 2012
Constipation(external link) BPAC, NZ, 2007
Continuing professional development
Podcast
Constipation in children(external link) Goodfellow Podcast, NZ, 2020
In this podcast, Dr Rebecca Hayman reviews the optimal management of childhood constipation. She discusses pathophysiology, the important clues that can be gained from a comprehensive history and thorough examination, and finally the management including dis-impaction, and why long term maintenance treatment is so important.
e-Learning Module
Idiopathic constipation and nocturnal enuresis in childhood – a guide to management: putting NICE guidelines into practice(external link) BMJ Learning
Resources
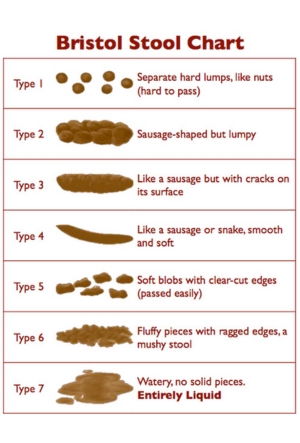
Bristol Stool Chart(external link)
Cochrane review
Laxatives for the management of childhood constipation (Plain language summary)
"Constipation within childhood is an extremely common problem. Despite the widespread use of laxatives by health professionals to manage constipation in children, there has been a long-standing lack of evidence to support this practice.
- This review included eighteen studies with a total of 1643 patients that compared nine different agents to either placebo (inactive medications) or each other.
- The results of this review suggest that polyethylene glycol preparations may increase the frequency of bowel motions in constipated children. Polyethylene glycol was generally safe, with lower rates of minor side effects compared to other agents. Common side effects included flatulence, abdominal pain, nausea, diarrhoea and headache.
- There was also some evidence that liquid paraffin (mineral oil) increased the frequency of bowel motions in constipated children and was also safe. Common side effects with liquid paraffin included abdominal pain, distention and watery stools.
- There was no evidence to suggest that lactulose is superior to the other agents studied, although there were no trials comparing it to placebo.
- The results of the review should be interpreted with caution due to methodological quality and statistical issues in the included studies. In addition, these studies were relatively short in duration and so it is difficult to assess the long-term effectiveness of these agents for the treatment of childhood constipation. Long-term effectiveness is important, given the often chronic nature of this problem in children." (Gordon M et al, Cochrane Review 2012)
Gordon M, Naidoo K, Akobeng AK, Thomas AG. Osmotic and stimulant laxatives for the management of childhood constipation(external link) Cochrane Database of Systematic Reviews 2012, Issue 7. Art. No.: CD009118. DOI: 10.1002/14651858.CD009118.pub2.
Apps
Nutrition apps – children