Sleep and children
Key points about sleep and children
- Sleep is important for restoring your child's energy and for their growth and development.
- If they don't get enough sleep, or their sleep is of poor quality, it can negatively affect their behaviour, learning, health, wellbeing and weight.

Signs your child or teenager is not getting enough sleep include:
- if they’re telling you they’re tired
- if they're appearing more irritable
- if they are napping during the day (for an older child) or falling asleep in inappropriate situations
- if it’s hard for them to get up and going in the morning
- if they are sleeping a lot more on the weekends than during the week, they are probably making up for ‘sleep debt’ and need help to get more sleep more during the week.
Video: Baby tired signs
This video may take a few moments to load.
(The Sleep Store, NZ, 2017)
The younger your child is the more sleep they need. It’s normal for children to have daytime naps until they are 3 to 5 years old. If they need naps past this age, they may not be getting enough sleep at night.
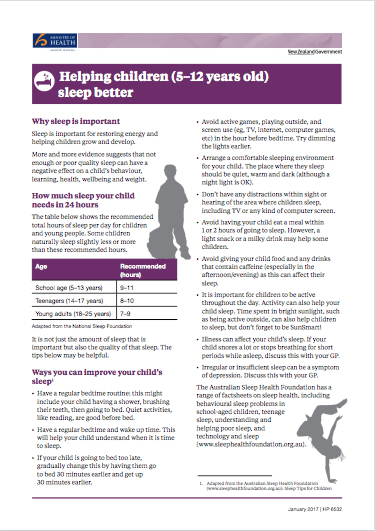
The normal range of sleep needed for babies through to teenagers is in the following table. Bear in mind that not every child's needs fit strictly within the age group recommendations.
Age and recommended hours of sleep needed per night
- Newborn (0–3 months) – 14 to 17 hours
- Infant (4–11 months) – 12 to 15 hours
- Toddler (1–2 years) – 11 to 14 hours
- Pre-schooler (3–4 years) – 10 to 13 hours
- Primary/intermediate school age (5–13 years) – 9 to 11 hours
- Teenagers (14+) – 8 to 10 hours
During the first weeks of life, your baby does not have a set day-night rhythm. You can help create this rhythm by setting regular times for going to bed and waking up. The more regular the hours, the stronger the sleep-wake cycle will be.
Other things you can do include:
- develop a bedtime routine – this helps signal that it’s time for sleep
- help your baby understand that night time is for sleep – don’t rush to your baby if they just stir, and keep the light and your voice low when you feed or tend them at night
- look out for the tired signs your baby may show
- get them used to being put into bed drowsy but awake
- help your baby learn to sleep on their own, although many will need some soothing to do this initially
- try to avoid creating sleep associations that are outside of the bed, eg, only rock or push them around in a stroller when really needed
- follow the SUDI guidance, including your baby having their own sleeping space and putting them to sleep on their back.
If you’ve tried all of this and your baby is still not sleeping, don’t blame yourself. Every baby develops at their own pace. Some babies are so-called great sleepers from an early age; others take years to establish settled sleep patterns. While it’s a good idea to help your baby establish good sleep routines, it’s important to attend to your own wellbeing as well. Plunket services can also be helpful to consult with. See also our tips on coping with sleep deprivation as a new parent.
The main thing to do is have a bedtime routine for your child and follow this consistently. This helps your child’s body and mind to enjoy the day and get ready for bed. They will go to sleep more easily if they go to bed at about the same time each night. They are also more likely to wake at about the same time each morning.
A bedtime routine starts with at least an hour away from screens, such as cell phones, tablets, computers and anything else that is too stimulating. It can be helpful to have household rules for technology that cover all members, eg, adults not using devices at a time when children are encouraged not to be.
A routine often includes a bath/shower, pyjamas, a drink, cleaning teeth, a toilet visit, a bedtime story, a goodnight kiss and then lights out as you leave the bedroom.
If your child has trouble going to sleep even after a regular routine is established:
- make sure they’re not going to bed too early or too late for them, and if so, adjust their bedtime by 15 minutes a night
- make sure there’s no noise disturbing them from the TV or other activity near their bedroom
- teach them how to use their breath to quieten their mind by focusing on slow breathing
- help them learn to sleep without you in the room, by leaving the room with the lights out before they fall asleep
- until it comes naturally, acknowledge good behaviour around sleep with praise and other rewards, eg, stickers
- try to make sure that your child only uses their bed for sleeping – lying on a bed and doing other activities (eg, watching a computer) makes it hard for their brains to associate their beds with sleep.
Make sure your child has plenty of physical activity every day. Include time outdoors, especially in the morning, so their body clock supports them being awake in daylight and asleep at night. Plenty of active play and other physical activities help your child to sleep well.
A full meal within an hour or two of bedtime can disrupt sleep, but a small snack near bedtime will help some children. Don’t give children food and drinks containing caffeine as this can make it harder for them to sleep.
Where possible, be consistent about your child going to sleep in the same place – don’t put them to sleep somewhere else and move them to their own bed later as this can be confusing for them when they wake up.
There are lots of cultural and practical variations about where children are best to sleep; the most important things are having a consistent and safe space. If you find that where your child is sleeping is different from most people you know, or it’s causing disruption in your family routine, you might wish to seek advice from a local professional you trust (eg, a Plunket nurse).
The following behaviours are common. You can help teach your child to change these habits so that they get a good night’s sleep every night. If your child has a sleep problem or condition, find out about other strategies.
Getting out of bed at bedtime
If your child can’t settle and comes out of their bed, stay calm and quiet, and take them back to bed. Get them to lie down and tell them to go to sleep and leave again. You can go back into the room on and off, for a short time. You may need to do this over and over. Each time, spend longer and longer out of the room. If it is more culturally appropriate for your child to sleep in your bed, these same steps can also apply to help them learn to fall asleep on their own.
Getting into your bed during the night
If you would like your child to be sleeping in their own bed and they come to your bed during the night, take them back to their own bed each time. Remember to remind them at bedtime that you expect them to stay in their own bed all night. Praise them in the morning when they do.
If your child is distressed about sleeping away from you, consider making a bed for them temporarily on the floor in your room so they can come and be close to you if they are scared (i.e. they still will have the consistency of sleeping in their own bed). Encourage them to sleep in their own bed but let them know there is a safe place they are welcome to come to if they need it.
Being scared of the dark
Reassure them that they are safe. Taking a soft toy to bed for comfort can help them feel less alone if they wake in the night. A small dim nightlight can also help. Be aware of what your child is reading and watching. Some children are more sensitive than others to intense or scary content and being exposed to this can lead to fear of the dark.
Bed wetting
Bed wetting at night is common with young children. However, most children will grow out of it. Treatment programmes are available for a child who has continued bed wetting. Find out more about bed wetting.
Teenagers are in a different stage of brain development that can affect their sleep cycles, with a tendency to fall asleep later. This can mean that a good sleep routine becomes even more important in this age group. Adults have a big influence on younger people in their household, so if you want your teenagers to have healthy sleep habits, it’s important that you model this behaviour.
Things you can do:
- eat well, be active, have some screen-free time and don’t stay up too late – and help your teenagers to do the same
- encourage them to do their homework earlier in the evening if possible so they don’t need to stay up late
- disconnect the wi-fi after a certain hour each night
- try to keep the weekend sleep and meal times similar to the weekdays (within a couple of hours).
The following links provide further information about sleep and children. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
KidsHealth(external link) NZ has a range of resources on sleep and children, including Sleep(external link), Sleeping sound(external link), Tools for managing sleep problems(external link), Sleep needs for teenagers(external link) and sleep and anxiety(external link)
Oriori (lullaby) lyric sheet(external link) and audio(external link) Ministry of Health, NZ
Sleep(external link) Healthy Kids, NZ
Australian Sleep Health Foundation(external link) has a range of factsheets on sleep health and children
Sleep and your baby(external link) Better Health, Australia, 2014
Sleep – children and naps(external link) Better Health Australia, 2014
Brochures
Ten tips to help your baby sleep better(external link) Sleep Health Foundation, Australia
Helping children (5-12 years old) sleep better [PDF, 151 KB] Ministry of Health, NZ, 2017
Technology and sleep(external link) Sleep Health Foundation Australia
Sit less, move more, sleep well: Active play guidelines for under-fives: Owhaowha (infants) 3 – 12 months. Ministry of Health, NZ, 2018 Available in the following languages: English(external link), te reo Māori(external link)
Sit less, move more, sleep well: Active play guidelines for under-fives: Tamaiti pūhou (babies) 0-3 months. Ministry of Health, NZ, 2018.Available in the following languages: English(external link), te reo Māori(external link)
Sit less, move more, sleep well: Active play guidelines for under-fives: Tamaiti nohinohi (toddlers) 1-2 years. Ministry of Health, NZ, 2018. Available in the following languages: English(external link), te reo Māori(external link)
Sit less, move more, sleep well: Active play guidelines for under-fives: Tamaiti (pre-school) 3-4 years. Ministry of Health, NZ, 2018. Available in the following languages: English(external link), te reo Māori(external link)
Apps/tools
Sleepio – sleep better(external link)
References
- Normal Sleep - Primary School Aged Children (external link)KidsHealth
- Addressing weight issues in young people and families in New Zealand(external link), BPAC, NZ, 2012
- How much sleep do we really need?(external link) Sleep Health Foundation, Australia, 2023
- Behavioural sleep problems in school-aged children(external link) Sleep Health Foundation, Australia, 2023
- Parenting Teens - Sleep Needs In Teenagers(external link) KidsHealth
A New Zealand study found that in children under 5 years, each extra hour of sleep a night led to a reduced BMI of 0.48 kg/m2 by age 7 years. Addressing weight issues in young people and families in New Zealand(external link) BPAC, NZ, 2012
Melatonin may be useful off-label for treating sleep disturbances in children with neurodevelopmental disorders. However, there is a lack of studies on the potential adverse effects of prolonged melatonin use, particularly in children and adolescents. Melatonin – is it worth losing any sleep over?(external link) BPAC, NZ, 2015
Oximetry(external link) Starship Clinical Guidelines, NZ, 2021
Sleep disturbances – managing parasomnias in general practice(external link) BPAC, NZ, 2012
See our page SUDI for healthcare providers
Brochures
Ministry of Health, NZ, 2017
Credits: Healthify Editorial Team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr David Chinn, child and adolescent psychiatrist; Tania Stanton, clinical psychologist; and Rewa Murphy, clinical psychologist
Last reviewed:
Page last updated:





