Sepsis
Key points about sepsis
- Sepsis is a life-threatening reaction of your immune system to an infection in your body.
- Sepsis can quickly cause multiple organ failure and death, so time matters.
- Get immediate medical help if anyone has any of the symptoms listed below.
- If you don't know what to do call Healthline 0800 611 116.

Video: Could this be sepsis? Dr Erik McClain
Symptoms of worsening infection require immediate medical attention. Time matters. If not treated quickly, sepsis can quickly lead to multiple organ failure (eg, liver, kidney or lung failure) and death.
Usually, the first symptoms are those associated with the source of infection, eg, a cough due to pneumonia (lung infection) or tummy pain from appendicitis. People with sepsis usually feel extremely unwell with 1 or more of the following symptoms.
Symptoms that indicate an infection is getting worse include:
- fever and shaking, chills, waves of hot and cold
- feeling very unwell or exhausted
- fast breathing or feeling very short of breath
- passing less urine (pee) than usual
- dizziness, or changes in mental alertness, eg, confusion, drowsiness or disorientation.
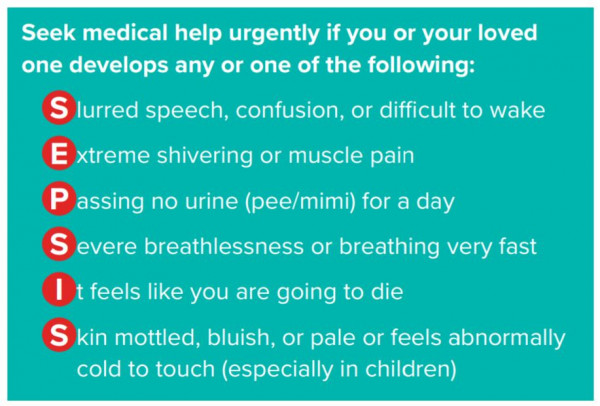
Image source: Have an infection? Just ask "could it be sepsis?" [PDF, 162 KB] Sepsis Trust, NZ
Call Healthline free on 0800 611 116 if you don't know what to do. Ask 'Could this be sepsis?'
What causes sepsis?
Sepsis is a condition caused by your body’s immune system responding abnormally to an infection, which can lead to tissue damage, organ failure and death. The infection can start anywhere in your body – it may be only in 1 part or it may be widespread. Your immune system usually works to fight any germs (bacteria, viruses, fungi) or to prevent infection. However, for reasons we don’t fully understand, sometimes the immune system goes into overdrive and starts to attack our organs and other tissues. Common infections leading to sepsis include the following (we’ve put the words that healthcare professionals use in brackets):
- chest infections (pneumonia)
- urine infections (urinary tract infection)
- leaks from the bowel (intra-abdominal sepsis)
- infections of skin (cellulitis), joint (septic arthritis) and bone (osteomyelitis)
- infection of the blood (bacteraemia) or heart (endocarditis).
Sepsis can lead to a drop in blood pressure which leads to your circulatory system being unable to provide enough oxygen and nutrients to the rest of your body. This leads to damage to various organs, eg, your lungs, heart, kidneys and brain. Multiple organ failure and death can result, especially if sepsis is not diagnosed early and treated quickly.
Sepsis is an emergency.
When sepsis is severe, you develop septic shock. This is when your blood pressure drops to a dangerously low level. This carries the highest risk of death and complications. Sepsis, especially if severe, needs urgent hospital treatment and may require admission to an intensive care unit (ICU). ICUs are able to support many affected body functions, eg, breathing or blood circulation.
Sepsis can occur at any age, but you're at increased risk if you have a serious infection or a weakened immune system, eg, if you:
- are very young or very old
- have a weak immune system (due to chemotherapy or taking immunosuppressant drugs, eg, prednisone, which make it easier to get an infection)
- have had an organ transplant and are on anti-rejection medicines
- have a long-standing (chronic) disease, eg, diabetes, chronic obstructive pulmonary disease (COPD) or kidney disease
- have severe liver disease
- have HIV or leukaemia
- have recently had surgery
- have wounds or injuries as a result of an accident
- have drips or catheters attached to your skin
- are pregnant or have just given birth.
Sepsis is a particular risk for people already in hospital because of another serious illness.
Sepsis and cancer
Having cancer and some treatments for cancer can put you at higher risk of developing an infection and, as a result, sepsis. This is because your body may not be able to fight off infections as it normally would.
- Although an infection can happen at any time, your risk of getting an infection is especially increased when you have very low levels of a certain type of white blood cell called neutrophils. This is known as neutropaenia.
- Your doctor will routinely test for neutropaenia by checking the level of your white blood cells (neutrophils). Read more about cancer, sepsis and infection.(external link)
Sepsis and pregnancy (also called maternal sepsis)
If sepsis develops during pregnancy, during or after giving birth, or after an abortion, it's called maternal sepsis. It's one of the main causes of maternal death. If you feel unwell at any time during your pregnancy, consult your healthcare provider.
Prevention is important for reducing your risk of getting sepsis. Make sure you attend recommended antenatal (pregnancy) visits, where healthcare providers will:
- screen you for common infections
- advise you on how to prevent infections
- provide information on vaccinations and nutrition
- prescribe treatments to prevent or treat bugs that may lead to infection in you or your baby.
The risk of having an infection after a Caesarean section (C-section) is 4 times higher than by vaginal birth. This is mainly related to the risk of developing an infection at the site of the wound. Seek immediate medical attention if you have any of the following within 14 days after giving birth:
- a fever
- an open wound or pus
- painful, red, swollen breasts with fever
- bad smelling discharge or pus from your vagina
- severe abdominal (tummy) pain
- pain when urinating (peeing) plus feeling unwell and having a fever.
Read more about maternal sepsis.(external link)
If you have sepsis, a A healthcare provider will see signs of an infection and 1 or more of the following:
- very low blood pressure
- very fast heart rate
- rapid breathing (25 breaths per minute or more)
- low levels of oxygen in your blood
- reduced level of consciousness (somebody responding only to voice or pain)
- high levels of lactic acid in the blood (indicating your body isn’t getting enough oxygen).
Sepsis can sometimes be hard to diagnose, especially early on. If you have an infection, or think you do, you should ask your healthcare provider if you could have sepsis.
If someone you care for is sick with an infection and/or fever, ask yourself the following questions:
- Are they confused or difficult to wake?
- Are they breathing very fast?
- Do their hands and feet feel cold or do they have mottled or splotchy skin?
- Are they passing a lot less urine (pee, mimi) for a day?
- Are they sicker than they’ve ever been before?
| If yes, call 111 and tell the operator and ambulance crew that you’re worried about sepsis. In other circumstances it may be appropriate to see your GP or urgent care provider and just ask – could it be sepsis?/he pātai – he sepsis tēnei? |
|---|
Treatment of sepsis depends on the site and cause of the infection, the organs affected and the extent of any damage.
It's very important to get treatment for sepsis as early as possible. That's why recognising the symptoms of sepsis and calling for help is so important.
After sepsis has been recognised there are 6 things that have to be done within 1 hour – this is called the 'Sepsis Six' bundle. In healthcare, a bundle is a group of treatments that reduce harm (or improve outcomes) when given together as a package. If everything in the Sepsis Six bundle is done within an hour (compared with no treatment), the chance of death from sepsis is roughly halved.
The Sepsis Six bundle steps are to:
- give antibiotics
- give fluids
- give oxygen (if required)
- take blood cultures (to try and grow the bug causing sepsis)
- take a blood lactic acid level (a ‘lactate’)
- take measurements of urine output (to make sure enough blood is flowing to the kidneys).
Apps reviewed by Healthify
You may find it useful to look at some Self-management and healthy living apps.
There has been some research into sepsis survivors which found that, over the following year at least, some of them are more likely to contract another infection. As with any infection, there's a risk of sepsis. But most people who’ve had sepsis before seek help early on and are treated promptly.
If you (or your loved one) have an infection, then you should keep a close eye for any signs of sepsis and seek help urgently if you're worried.
Most people who survive sepsis recover completely, but for some, full recovery may take a long time. Because you have been seriously ill, your body, mind and spirit need time to recover. As your body heals, you will get your strength back and, for most people, many of the problems described below will go away with time.
The early recovery phase
After you've had sepsis, it’s important to increase your level of activity slowly. Recovery involves rehabilitation to help restore you back to your previous level of health or as close to it as possible. Rehabilitation usually starts in the hospital where staff will assist you to move around and with your personal care such as bathing and dressing. This process or recovery and rehabilitation often requires a stay in hospital of about 7 days.
When you get home
As your body is still recovering, it's not unusual to experience the following symptoms when you get home:
- feeling tired – which can be general tiredness to extreme weakness and fatigue
- general body aches and pains
- difficulty moving around
- problems sleeping
- weight loss, lack of appetite, food not tasting normal
- dry and itchy skin that may peel
- brittle nails or hair loss.
Having sepsis can be quite traumatic, so it's also not unusual to feel emotionally stretched, including:
- feeling unsure of yourself
- not caring about your appearance
- wanting to be alone, avoiding friends and whānau
- having flashbacks, bad memories
- being confused about what's real and what isn’t
- feeling anxious, more worried than usual
- having poor concentration
- having low mood and being depressed, angry or unmotivated
- feeling frustrated at not being able to do everyday tasks.
If you find it difficult to cope, talk to your healthcare provider. They know that this can happen after sepsis and they can help you to get through these feelings and frustrations.
How can I help myself recover at home?
People who leave hospital after sepsis often struggle to return to their previous level of function. The main problems directly related to sepsis are physical, cognitive (relating to brain function) and psychological.
Each person will recover at their own pace. Set small, achievable goals for yourself to do each day, eg, taking a bath, getting dressed or walking up the stairs. Here are some tips to help you on your road to recovery:
- take all the antibiotics or other medicines you may have been sent home with
- rest and rebuild your strength
- eat a balanced diet
- exercise as you feel up to it
- talk about what you are feeling with family and friends
- record your thoughts, struggles and milestones in a journal
- learn about sepsis to understand what happened
- ask your family to fill in any gaps you may have in your memory about what happened to you
- make a list of questions to ask your healthcare provider when you go for a check-up.
Are there any long-term effects of sepsis?
People who survive sepsis usually recover completely and their lives return to normal. However, as with some other illnesses requiring intensive medical care, some people have long-term effects. These may not become apparent for several weeks after you've had sepsis and may include:
- sleep problems, eg, difficulty getting to or staying asleep (insomnia), nightmares or vivid hallucinations
- panic attacks
- severe muscle and joint pains
- decreased mental (cognitive) functioning
- loss of self-esteem and self-belief
- problems with the functioning of your organs, eg kidney failure, lung problems, etc.
- in rare cases, loss of hands, arms, legs or feet (limb amputation).
If you feel that you're not getting better or finding it difficult to cope, talk to your healthcare provider. Talk to your employer about a graduated return to work if that is possible. Remember that sepsis is a severe illness, like a heart attack or a stroke, and many people with these conditions can't go straight back to work.
Sepsis stems from an infection, so by treating any infection seriously, you'll decrease the chances of developing sepsis. This means seeking early treatment and taking antibiotics when prescribed. You can also prevent infections by:
- frequent and thorough hand washing
- getting vaccinated for the seasonal flu (and COVID-19) each year
- coughing into your elbow, not your hand (to help prevent spreading infection if you're sick)
- maintaining a healthy lifestyle with nutritious food, exercise and plenty of sleep.
The following links have more information about sepsis. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
What is sepsis?(external link) Sepsis Trust NZ
Sepsis – Information for patients, family and whānau(external link) Sepsis Trust NZ
Sepsis(external link) Centers for Disease Control and Prevention, US
Sepsis(external link) NHS Choices, UK
Sepsis – FAQ(external link) World Sepsis Day
Life after sepsis(external link) Australian Sepsis Network
Apps
Self-management and healthy living apps
Resources
Have an infection? Just ask "could it be sepsis?" [PDF, 162 KB] Sepsis Trust, NZ. Also available in te Reo Māori(external link)
Cancer, infection and sepsis fact sheet(external link) Centers for Disease Control and Prevention, US
References
- Sepsis care and treatment in NZ and Australia(external link) Journal of Emergency Medicine, 2017
- Infection and antibiotic use following major surgery(external link) HQSC, NZ
- Patient deterioration and sepsis(external link) HQSC, NZ
Sepsis is one of the most serious conditions we can see as health professionals and with a mortality rate of 10 to 20%, we need to recognise it immediately and act fast.
Because it doesn't fall neatly into one specialty, the extent of the problem hasn't been profiled as clearly as other serious conditions, yet each year it kills more people than lung, breast and bowel cancer combined.
To address this gap, a group of clinicians at Waikato Hospital have set up Sepsis Trust NZ and adapted the NICE guidelines for New Zealand. This page highlights some of the key messages from these documents and viewers should read the full versions for more detail.
Clinical tools and guidelines
Clinical tools (adapted for New Zealand)
Paediatric sepsis screening and action tool [PDF, 1.5 MB]
Adult sepsis screening and action tool [PDF, 1.4 MB]
Maternal sepsis screening and action tool [PDF, 1.6 MB]
Sepsis hypoperfusion pathway [PDF, 694 KB]
Empiric antibiotic guidance [PDF, 115 KB]
For more resources, visit Sepsis Trust NZ(external link)
Patient deterioration and sepsis factsheet(external link) Health Quality & Safety Commission NZ
Sepsis – recognition, diagnosis and early management(external link) BPAC NZ and NICE guidelines
Goodfellow unit short course (30 mins)
Could this be sepsis?(external link) Goodfellow Unit, NZ, 2024
Apps
Brochures
Have an infection? Just ask "could it be sepsis?"
Sepsis Trust, NZ
English, te reo Māori
Sepsis – Information for patients, family and whānau
Sepsis Trust NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:






