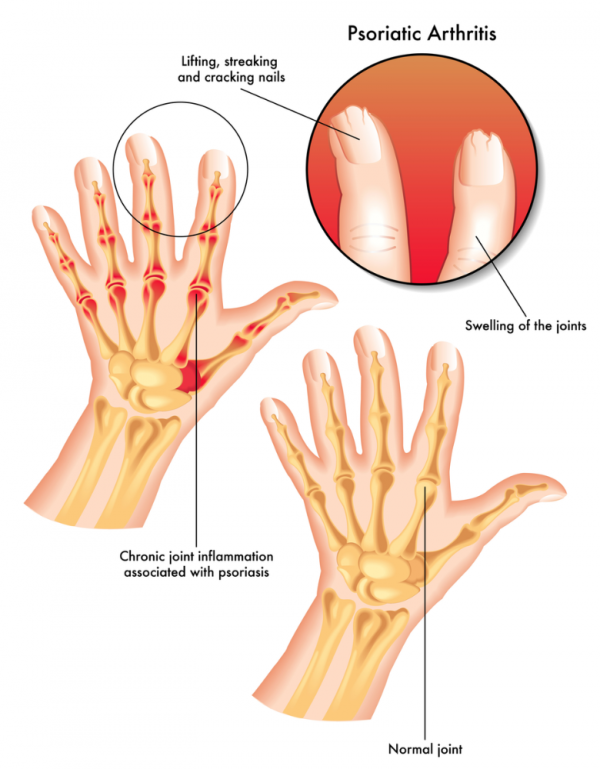
Psoriatic arthritis is a type of inflammatory arthritis linked to psoriasis, a skin condition with red, scaly patches of skin. The tissues around your joints, which are called the synovium, get inflamed causing pain, stiffness and swelling. It can affect any joint, but it’s most common in your fingers, feet, toes, knees and sometimes your spine. Your tendons and ligaments can also get inflamed.
Psoriatic arthritis usually develops in people who already have psoriasis, but it can also appear before the skin rash develops. Up to 3 in 10 people with psoriasis get psoriatic arthritis, usually within 10 years of the psoriasis first appearing. It can happen at any age, most commonly between the ages of 25 and 50. It's equally common in men and women.