A pressure sore is an area of damaged skin and tissue often caused by staying in one position for too long. If you are sitting up in bed, sliding down can injure your bottom and heels. Prolonged pressure on an area of your skin stops the blood flow to that area. This cuts off the oxygen supply and causes skin cells to die.
Having a pressure sore can have a huge impact, both for the patient and their carer. It can cause pain and discomfort, feelings of anger and blame, and reduce quality of life through infection, delayed healing, altered body image and low mood. The human toll on patients, carers and their families/whānau should not be underestimated. Having a pressure sore also carry connotations of neglect and mismanagement on the part of carers and health professionals.
Love our website? We do too. Did you know we're a charity? Donate now to help us keep it free for everyone in Aotearoa New Zealand.
Pressure sores
Also called bed sores, pressure sores, pressure areas, pressure ulcers or a pressure injury
Key points about pressure sores
- Pressure sores are also known as pressure injuries, pressure ulcers, bed sores or pressure areas. They're caused by staying in one position for too long, such as prolonged sitting or lying.
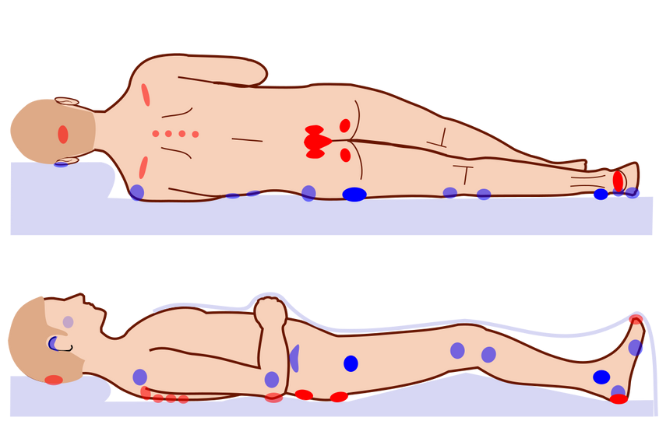
- They usually form around bony areas of your body, such as your ankles, heels, hips and tailbone.
- They can develop in a matter of hours. The first sign of a pressure sore is usually a discoloured skin area that doesn't turn white when pressed.
- The main complication of a pressure sore is an infected wound. See your doctor immediately if you have any signs of infection.
- There are things you can do to prevent pressure sores and, if you do get one, there is a range of treatment available.
You are at risk of a pressure sore if you are unable to move around or change position easily, such as if you:
- spend long periods of time in bed
- sit in a wheelchair or chair for long periods
- are immobile due to a serious illness or have just had a major surgery
- are elderly or frail with thin fragile skin
- have skin that is often wet from sweat, urine (pee) or bowel movements (poo)
- have damp skin due to sweating
- cannot feel pain or pressure on an area of your skin (due to stroke, diabetes, spinal cord injury or epidural).
A pressure sore usually forms around bony parts of your body, such as your ankles, heels, hips and tailbone, as these areas take the weight of your body.
| Description | Image |
|
On your back |
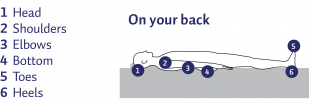 |
|
On your front |
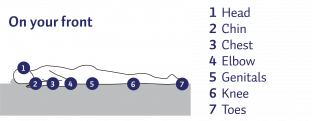 |
|
On your side |
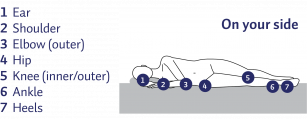 |
|
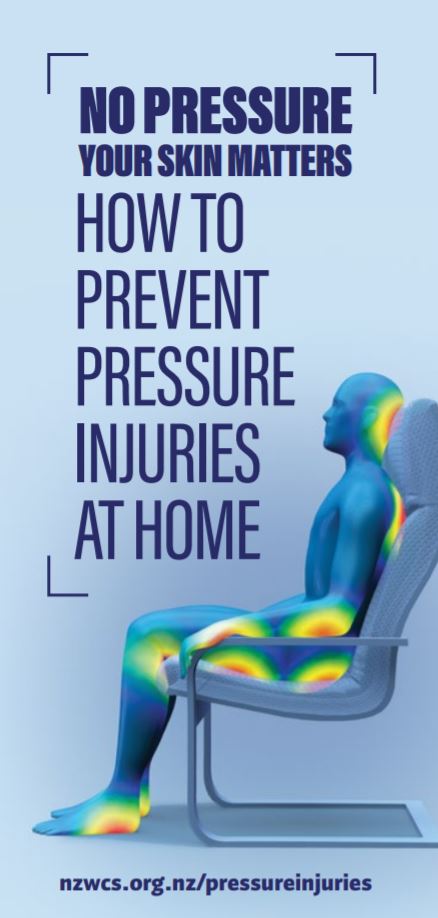
Sitting up |
 |
Image credit: How to prevent pressure injuries at home(external link)
Pressure sores can develop in a matter of hours. The first sign is usually a discoloured area on your skin that doesn't turn white when you press on it. The injured skin may get progressively worse and eventually lead to an open wound. Other symptoms include:
- pain, tenderness or itchiness on your skin
- swelling
- reddened skin
- blisters
- pus draining out from the affected area
- the skin being hotter or colder than other areas of your skin.
Your doctor or nurse will diagnose a pressure sore by examining your skin. They will establish how severe it is to determine what treatment is best for you. If they think the pressure sore is infected, they may take a swab around your skin to find out the cause of the infection.
Daily checks are needed to look for early warning signs such as red, purple or blue torn or swollen skin, especially over bony areas, or for signs of infection, such as skin warmth, swelling, cracks, calluses and wrinkles.
You may need care from a team of health professionals such your GP, a nurse specialising in wound care, an occupational therapist, a physiotherapist, a dietitian taking care of your diet, a skin specialist or a plastic surgeon, depending on your condition. They are involved in different aspects of your wound care. Treatment may include:
- reducing pressure on the affected skin by changing position frequently and using pressure-redistributing devices such as pressure-relieving mattresses and cushions
- prescribing medications to control pain or itchiness
- dressings such as gel and foam-based dressings
- taking care of the wound by keeping your skin clean and dry
- maintaining good nutrition and hydration as a poor diet can slow the healing of a pressure sore
- preventing complications such as infections.
If you have a large, deep sore that doesn't heal properly, your doctor may need to remove damaged tissue by surgery.
If you have a pressure, it is important to get it treated as soon as possible, If left untreated, you are at risk of developing infections such as cellulitis, sepsis or bone and joint infections.
| See your doctor immediately if you have any signs of infection such as fever and chills, a sore that drains pus, smelly wound, increased redness, temperature or swelling around your sore. |
Most pressure sores are preventable. It is much better to prevent pressure sores than to treat them.
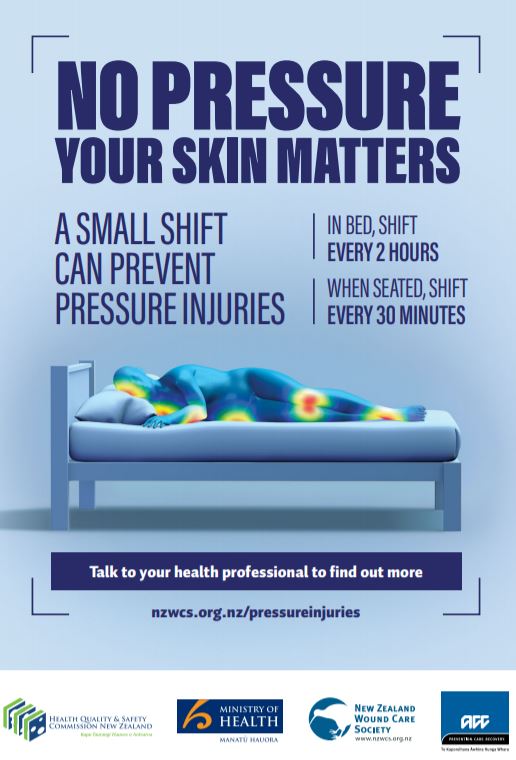
If you are in bed:
- change position every 2 or 3 hours – even a small shift in position can help
- use pillows to stop your knees and ankles touching each other, particularly when lying on your side
- try to avoid creases in your bed linen
- if sitting up in bed, be aware that sliding down can cause injury to your bottom and heels
- ask for help if you need it.
If you are seated:
- relieve pressure by leaning forward or leaning side to side for a few minutes every half hour
- if you can stand, stand for a few minutes
- if you can walk, go for a short walk.
Here are 5 tips to prevent pressure sores.
Change position frequently

One of the best ways to prevent pressure sores is to reduce or relieve direct pressure on the areas at risk by moving around and changing position as much as possible. People who spend most of their time in bed are advised to change position every 2–3 hours, even during the night. People who use a wheelchair are advised to shift position within their chair about every 15 minutes, by leaning forward or moving side to side. If you can't move, ask your carer to reposition you regularly.
Don't drag your heels or elbows when moving
Don't drag your heels or elbows when moving in your bed or chair. Chafing or friction caused by your skin rubbing against the sheets or other surfaces can remove top layers of skin and cause pain. Instead its best to lift your limbs up. If you are unable to do this, ask your carer for help.
Use pillows, cushions or special mattresses
 Using pillows or cushions as soft buffers between your skin and the bed or chair can be helpful. No two skin surfaces should rest against each other, eg, while lying in bed, place a pillow between your knees and ankles to prevent them from touching each other. If you are confined to bed, ask your healthcare provider about the use of heel and knee protectors or pressure relieving mattresses.
Using pillows or cushions as soft buffers between your skin and the bed or chair can be helpful. No two skin surfaces should rest against each other, eg, while lying in bed, place a pillow between your knees and ankles to prevent them from touching each other. If you are confined to bed, ask your healthcare provider about the use of heel and knee protectors or pressure relieving mattresses.
Take care of your skin
Taking care of your skin and doing regular skin checks are important in preventing pressure sores. Check your skin at least once a day for redness, changes in colour, blisters, bruises, cracked, scraped or dry skin. Closely inspect areas that are at especially high risk for pressure sores. The highest risk is where your bones are close to the surface and your skin is directly over bone. Use a mirror to inspect skin in hard-to-see areas or ask your caregiver to help you. If you notice a discolored area, stay off the area until it returns to normal skin colour.
Keep your skin at the right moisture level, as damage is more likely to occur if your skin is either too dry or too moist. Use moisturising products to keep your skin supple and prevent dryness, but avoid massaging bony areas where the skin is too delicate. Immediately wash and dry skin and change clothing after any leakage of stool (poo) or urine (pee). Avoid harsh soaps, skin agents with alcohol and antibacterial or antimicrobial soaps.
Eat healthily and drink plenty of fluids
Eating a healthy and nutritious diet and preventing dehydration by drinking enough liquid is important in preventing pressure sores. Being obese or having severe weight loss can increase the risk of getting pressure sores. A poor diet can affect the health of your skin and your immune system. Likewise, hydration plays a vital role in your skin's health and helps to repair injured skin. Adequate fluid intake is necessary for wound healing, to support the blood flow to wounded areas and to prevent breakdown of your skin.
|
Stories |
|
Rosalie Ross Cunningham’s story(external link) In 2012, Rosalie Ross Cunningham passed away due to sepsis caused by an |
|
John Rankin’s story (hospital)(external link) In 2016, John Rankin was diagnosed with lymphoma after being admitted to hospital. |
|
Amanda Bradbury's story (hospital and community)(external link) In 2013, Amanda Bradbury was admitted to hospital with lymphedema (swelling) in her legs and a pressure injury on her sacrum, believed to be caused by an old, ill-fitting wheelchair. |
|
David Jackson (hospital)(external link) In March 2017, David Jackson underwent a bilateral (double) hip replacement. |
For more patient stories, visit Pressure injury prevention – patient stories(external link) Health Quality & Safety Commission, NZ
Videos about pressure injury prevention
Video: Shelley Roberts, Menzies Health Institute Qld, pressure injury prevention
This video may take a few moments to load.
(Griffith Health, Australia, 2017)
1. Video: WOF
This video may take a few moments to load.
(NZ Spinal Trust, 2018)
2. Video: Skin checks
This video may take a few moments to load.
(NZ Spinal Trust, 2018)
3. Video: Pressure relief
This video may take a few moments to load.
(NZ Spinal Trust, 2018)
4. Video: Gear
This video may take a few moments to load.
(NZ Spinal Trust, 2018)
5. Video: Nurse Bev
This video may take a few moments to load.
(NZ Spinal Trust, 2018)
6. Video: Awareness
This video may take a few moments to load.
(NZ Spinal Trust, 2018)
The following links provide further information about pressure sores. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
How to prevent pressure injuries at home(external link) NZ Wound Care Society, Ministry of Health NZ, ACC NZ & Health Quality & Safety Commission NZ
Pressure injury prevention and treatment(external link) NZ Spinal Trust
Pressure ulcer(external link) DermNet, NZ
Bedsores (pressure ulcers)(external link) Mayo Clinic, US
Helping prevent pressure injuries(external link) ACC, NZ
Resources
How to prevent pressure injuries at home. New Zealand Wound Care Society, Ministry of Health, Health Quality & Safety Commission & ACC, NZ Available in the following languages: English(external link), Arabic(external link), Burmese(external link), Hindi(external link), Korean(external link), te reo Maori(external link), Punjabi(external link), Samoan(external link), Simplified Chinese(external link), Spanish(external link), Tagalog(external link), Tokelauan(external link), Tongan(external link), Traditional Chinese(external link), Tuvaluan(external link)
No pressure your skin matters. New Zealand Wound Care Society, Ministry of Health, Health Quality & Safety Commission and ACC, NZ Bed(external link), Chair(external link)
References
- How to prevent pressure injuries at home(external link) NZ Wound Care Society, Ministry of Health NZ, ACC NZ & Health Quality & Safety Commission NZ
- Pressure ulcer(external link) DermNet, NZ
- Pressure injury prevention(external link) Health Quality & Safety Commission NZ
- The care for a quality improvement programme to reduce pressure injuries in NZ(external link) KPMG, NZ, 2016
- Skin care and pressure sores(external link) University of Washington, US, 2009
- Prevention and treatment of pressure ulcers/injuries – clinical practice guideline(external link) International Guideline, 2019
- How to classify and document pressure injury [PDF, 349 KB] NZ Wound Care Society, HQSC, NZ, ACC, NZ & Ministry of Health, NZ, 2019
- Guiding principles for pressure injury prevention and management in NZ(external link) HQSC, NZ, ACC, NZ & Ministry of Health, NZ, 2017
- Pressure injury prevention(external link) Waitematā DHB, NZ
- Microbiological assessment of infected wounds – when to take a swab and how to interpret the results(external link) BPAC, NZ, 2013
- Helping prevent pressure injuries(external link) ACC, NZ, 2021
- Pressure injury in spinal cord injury – consensus statement(external link) ACC, NZ, 2021
- Repositioning for pressure injury prevention in adults(external link) Cochrane Database of Systematic Reviews, 2020
- Wound care – a guide to practice for healthcare professionals(external link) Ausmed Australia
- Prevention and treatment of pressure ulcers – quick reference guide(external link) National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel & Pan Pacific Pressure Injury Alliance, 2014
Brochures
New Zealand Wound Care Society, Ministry of Health, Health Quality & Safety Commission & ACC, NZ
Arabic, Burmese, English, Hindi, Korean, te reo Māori, Punjabi, Samoan, Simplified Chinese,Spanish, Tagalog, Tokelauan, Tongan, Traditional Chinese, Tuvaluan
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Rachel Fluke, Delivery Lead - Pressure Injury Programme, ACC
Last reviewed:
Page last updated: