Peptic ulcer
Key points about peptic ulcers
- Peptic ulcers are small holes in the lining of your stomach or gut.
- They are mainly caused by a bacterial infection or from anti-inflammatory medicines.
- Seek advice from a healthcare provider if you have a peptic ulcer.
- If peptic ulcers aren't treated, they can be very uncomfortable and can cause serious problems, eg, internal bleeding.
- Treatment includes treating the cause of the ulcer, taking medicines to reduce stomach acid levels and reviewing any medicines you take for pain relief.
- Stopping smoking, having regular healthy meals and avoiding triggers (eg, coffee, alcohol) can help reduce your symptoms.

Video: How a peptic ulcer develops
This video may take a few moments to load.
(Bupa Health UK, 2013)
The most common symptom or sign of an ulcer is pain in the abdomen. It often starts within a few hours of eating. Other symptoms include:
- bloating or feeling full or gassy
- indigestion, heartburn or acid reflux
- intolerance to fatty foods
- nausea (feeling sick) or vomiting (being sick)
- extreme weakness or dizziness
- weight loss.
In some people ulcers may bleed or perforate (make a hole in the stomach or the duodenum so food and bacteria go into the abdomen) or the area around them may become scarred, blocking up the intestines.
As well as seeking help from a healthcare professional, there are things you can do to care for yourself:
- Eat a well-balanced diet and have regular meals.
- Eat smaller meals and eat your evening meal 3–4 hours before going to bed.
- Identify and avoid food and drinks that make the pain worse (eg, alcohol, coffee, spicy food)
- Antacids can offer short term relief and may help protect the lining of the stomach. You can buy antacids from your local pharmacy.
- Stop smoking.
Apps reviewed by Healthify
You may find it useful to look at some Nutrition, exercise and weight management apps and Quit smoking apps.
There are two main types of peptic ulcer, named according to their location.
- Stomach ulcers are ulcers in the stomach. They are also called gastric ulcers.
- Duodenal ulcers are ulcers in your duodenum (the first part of your small intestine).
Peptic ulcers can also occur in your oesophagus (the tube that carries food and liquid from your throat to your stomach).
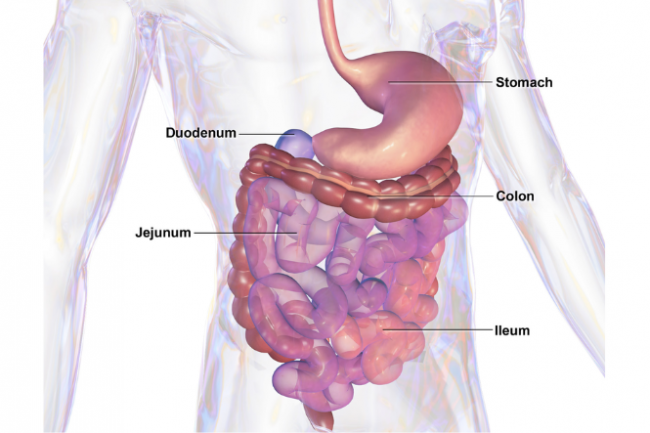
Image credit: blausen.com wikimedia commons
The most common causes of peptic ulcers are bacterial infection and long-term use of non-steroidal anti-inflammatory medicines (NSAID).
Bacterial infection
The majority of peptic ulcers are caused by infection with a bacteria called Helicobacter pylori (H. pylori). Most people with H. pylori infection don't have symptoms of peptic ulcer. The H. pylori bacteria make a substance that damages the mucous lining of the stomach so it can be damaged by acids that break down food during digestion. The bacteria also make the body produce more acid which makes the problem even worse. Read more about H. pylori.
Non-steroidal anti-inflammatory medicines (NSAID)
After H. pylori, the next most common cause of ulcers is taking long term or high dose anti-inflammatory medicines, eg, aspirin, ibuprofen or other non-steroidal anti-inflammatory drugs (NSAIDs). These can work in the same way as a bacterial infection, leaving your stomach open to attack from digestive acids. If you are taking anti-inflammatory drugs long term for pain relief you should talk to your healthcare provider about how you can protect yourself from developing ulcers.
Other causes
- Smoking increases your risk of developing ulcers and slows the healing if you have one.
- Increase in age.
- Family history of peptic ulcers especially if there is a family history of H.pylori infection.
- Crohn’s disease (an inflammatory disease of the intestines).
See your healthcare provider if you have peptic ulcer symptoms of a peptic ulcer. They may want to test if you have H. pylori infection (with a faecal antigen test or breath test) and you may need further tests such as an X-ray of your stomach and gut or an endoscopy/gastroscopy (to look inside your stomach).
Treatment for your ulcer will depend on what caused it. Medication treatment options include:
- Antacid medicines which can offer short term relief and may help protect the lining of your stomach. You can buy antacids from your local pharmacy.
- Medications to reduce the amount of acid produced in the stomach. These are called proton pump inhibitors.
- Medications to protect the lining of the stomach from further damage.
- Antibiotic medicines to treat H. pylori infection. Read about H. pylori and how it's treated.
- A review of safe treatments for pain relief if you have pain.
With treatment, most ulcers heal in a few months. They can return, but they're less likely to come back if you complete your course of treatment and make appropriate lifestyle changes.
Sometimes peptic ulcers can involve cancer and a repeat gastroscopy may be done to check that the ulcer is healing.
The following links provide further information about peptic ulcers. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Stomach ulcers(external link) NHS, UK
Peptic ulcer – a patient's guide(external link) Family Doctor NZ
Peptic ulcers(external link) Auckland Gastroenterology Associates, NZ
Apps
Nutrition, exercise and weight management apps
Quit smoking apps
References
- Peptic ulcer disease(external link) BMJ, UK, 2022
- Stomach and duodenal ulcers (peptic ulcers)(external link) John Hopkins Medicine, US
- Managing dyspepsia and heartburn in general practice – an update(external link) BPAC NZ, 2011
- H. pylori – who to test and how to treat(external link) BPAC, NZ, 2022
- Peptic ulcer – symptoms and causes(external link) Mayo Clinic, US
Managing dyspepsia and heartburn in general practice – an update(external link) Best Practice Journal (BPJ) and Best Practice Advisory Centre NZ, 2011
H. pylori – who to test and how to treat(external link) BPAC, NZ, 2022
Apps
Nutrition, exercise and weight management apps
Quit smoking apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Derek JY Luo, MBChB (Otago) FRACP, Consultant Gastroenterologist
Last reviewed:
Page last updated:





