If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Pelvic inflammatory disease
Also known as PID
Key points about pelvic inflammatory disease
- Pelvic inflammatory disease (PID) is an infection of the female upper reproductive organs in your pelvis.
- It’s most commonly caused by a sexually transmitted infection (STI), but other bacteria from your vagina or nearby organs can also cause PID.
- Common symptoms include lower abdominal (tummy) pain, abnormal vaginal bleeding or discharge, pain during sex, and fever, nausea or vomiting.
- Early treatment of PID is important to reduce the risk of serious complications, such as long-term pain and infertility.
- PID is treated with antibiotics and it's important that you complete the full course of treatment.

Pelvic inflammatory disease is an infection of the female reproductive organs – your uterus (womb), fallopian tubes, ovaries and the surrounding tissues.
It can be sexually transmitted or you may get it after surgery or having an IUD inserted, or after childbirth or termination of a pregnancy.
It’s important to treat PID as soon as possible to reduce the risk of complications such as infertility, ectopic pregnancy (a pregnancy outside your womb) and chronic (long-term) pelvic pain.
PID is common in young women (under 25 years) because chlamydia and gonorrhoea are common in this age group.
Most cases of pelvic inflammatory disease (PID) are caused by bacteria that spread from your vagina and cervix (the neck of your womb) to your uterus (womb), fallopian tubes and ovaries.
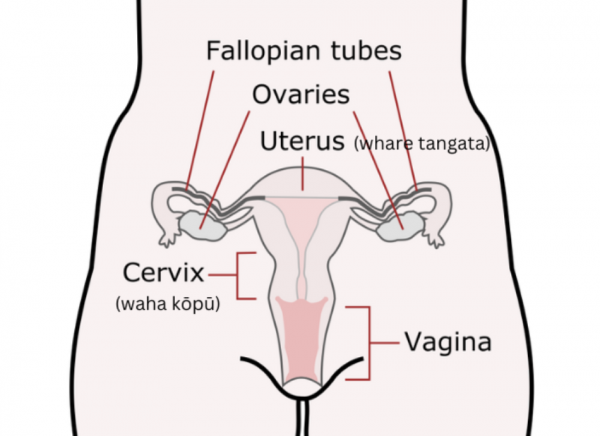
Image credit: open clipart (label added)
Many different types of bacteria can cause PID. The most common of these is an STI such as chlamydia and gonorrhoea.
Other less common causes include:
- after a termination of pregnancy (abortion) procedure
- after pelvic operations
- after insertion of an intrauterine device (IUD)
- in the first few weeks after delivery of a baby
- from spread of infections from nearby organs, eg, appendicitis.
You're more likely to get PID if you are younger than 30 years of age and/or if you have:
- unprotected sex without a condom
- a sexual partner with an STI
- had a new sexual partner in the past 3 months
- more than 1 sex partner or have a sex partner who has other sex partners
- had an STI in the past 12 months
- had PID before
- done vaginal douching
- had an IUD insertion (the small increased risk is usually within the first 3 weeks after the insertion)
- had a termination of pregnancy, miscarriage or childbirth, though the risk from these is very small.
The symptoms can vary from very mild to severe. Some people don't have any symptoms.
The most common symptoms are:
- pain or tenderness in your lower abdomen (tummy)
- abnormal vaginal discharge
- unusually heavy or painful periods
- unusual vaginal bleeding such as after sex or between periods
- pain during or after sex
- fever
- nausea or vomiting.
If you have the following symptoms, contact your healthcare provider or go to the nearest emergency department immediately as they may indicate severe PID:
- Severe tummy pain.
- Fever and chills.
- Repeated episodes of vomiting where it's hard to keep anything down.
- Unusually heavy vaginal bleeding that isn't stopping.
There's no specific, single test for pelvic inflammatory disease (PID). Your healthcare provider will rely on your symptoms and a physical examination to make a diagnosis. If you think you might have PID, tell your doctor or nurse.
- They’ll ask you about your symptoms, including your period, any previous operations you’ve had and whether you have a sexual partner who has a sexually transmitted infection for PID. They will also examine your abdomen (tummy) and, with your consent, do a vaginal (internal) examination. Read more about informed consent.
- Your healthcare provider will also do blood tests, a urine (pee) test and a vaginal swab to check for the cause of your infection. Your swab test can be negative for STIs even if you have PID.
- If you have PID, your healthcare provider will recommend that you have a sexual health check to check for other STIs such as HIV.
- If your symptoms are severe, or if you have any complications, your healthcare provider will ask for an ultrasound scan of your abdomen or other investigations.
- If there's a chance you might be pregnant and you have new-onset abdominal pain, you'll have a urine pregnancy test and if this is positive you'll have an ultrasound to check for ectopic pregnancy.
If your healthcare provider thinks it's very likely you have PID, you will be given a course of antibiotics, usually before test results come back. This is because it's important to treat PID as soon as possible to lower your risk of long-term complications.
A combination of antibiotics is used to treat PID as it's usually caused by a number of different bacteria. The treatment usually includes a single antibiotic injection (given into your buttocks) and antibiotic tablets for 2 weeks.
- Make sure you finish the full course of treatment, even if your tests are all clear and you're feeling better.
- If your symptoms don't improve or get worse within 2 to 3 days of treatment see your healthcare provider again.
- Return to your healthcare provider or clinic for a follow-up check after treatment.
- To prevent reinfection, don't have sex again (or use condoms if that's not possible) for 2 weeks from the start of your treatment and until any sexual contacts have been tested and treated.
If you have severe PID, your healthcare provider may refer you to the hospital to have medicines intravenously (through a drip in your arm).
If you have an IUD, it can be left in during treatment. However, your healthcare provider may remove it if you don’t respond to treatment after 2 to 3 days or if there is a high risk of you getting PID again.
If you have PID, it’s important to take your antibiotic treatment as instructed by your healthcare provider and to take the full course of treatment. You should rest, and if you have abdominal pain you can take pain relief, such as NSAIDs or paracetamol.
Return to your healthcare provider or clinic for a follow-up check after treatment (usually within 3 days, and again after 1 to 2 weeks). Reinfection is common so have a sexual health check after 3 months.
The complications of pelvic inflammatory disease (PID) get worse with repeated infections, so prevention of PID is very important.
Most PID in young women is the result of a sexually transmitted infection (STI).
- You can prevent STIs by using a condom every time you have sex, especially when having sex with new partners. Read more about safer sex.
- Make sure your sexual partners/contacts are tested and treated. Advise your sexual partner(s) from the past 3 months to get a sexual health check. You can talk to your healthcare provider for advice and information on how to talk to, and contact, those you’ve have sexual contact with. It’s important that they’re contacted so they can get tested and treated too (if needed) – even if they don’t have any symptoms they may still be infected and can pass the infection on or develop complications themselves.
- Have an STI check before any gynaecological procedure such as an IUD insertion or termination of pregnancy.
- Prompt treatment of STI may help prevent PID.
- Have regular STI check-ups if you change your sexual partner.
If you get PID more than once you’re at greater risk of developing long-term complications. You’re also more likely to have complications if your PID isn’t treated, or if treatment is delayed or you have a severe infection.
The complications of PID include:
- chronic or long-term lower abdominal pain
- scarring of your fallopian tube, which can cause infertility (difficulty getting pregnant) or ectopic pregnancy (pregnancy outside your womb)
- an abscess (collection of pus) in or around your fallopian tube and/or ovary. This can sometimes require surgery and a long course of antibiotics to treat.
In many countries, PID is the most common preventable cause of infertility.
To reduce the risk of these complications, it’s important to use condoms to prevent PID and to make sure your sexual partners or contacts are tested and treated too.
Pelvic inflammatory disease(external link) Sexual Wellbeing Aotearoa, NZ
Pelvic inflammatory disease(external link) Just The Facts, NZ
Brochures
Pelvic inflammatory disease(external link) Auckland Sexual Health Services, Health New Zealand | Te Whatu Ora, NZ
A guide to pelvic inflammatory disease(external link) British Association for Sexual Health and HIV, UK
Should I have a sexual health check?(external link) Health New Zealand | Te Whatu Ora, NZ
Chronic pelvic pain(external link) The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
Pelvic inflammatory disease (PID)(external link) Just the Facts, NZ
A compact guide to sexual health(external link) HealthEd, NZ
References
- Pelvic inflammatory disease(external link) Auckland Regional HealthPathways, NZ, 2023
- Pelvic inflammatory disease(external link) Aotearoa New Zealand STI Management Guidelines for use in Primary Care, NZ
- Pelvic inflammatory disease(external link) Auckland Sexual Health Services, Health New Zealand | Te Whatu Ora, NZ, 2020
- Partner notification and contact tracing(external link) Aotearoa New Zealand STI Management Guidelines for use in Primary Care, NZ, 2021
Sexual and reproductive health(external link) Health New Zealand | Te Whatu Ora
Pelvic inflammatory disease – a review(external link) O&G Magazine, 2019
Sexual health – best practice guidelines(external link) Sexual Health Society, NZ
Pelvic inflammatory disease(external link) NZSHS
Chronic pelvic pain in women(external link) BPAC, NZ, 2015
"A how-to guide" for a sexual health check-up(external link) BPAC, NZ, 2013
Brochures
HealthEd, NZ, 2019
RANZCOG, 2022

Pelvic inflammatory disease
Auckland Sexual Health Services, Health New Zealand | Te Whatu Ora, NZ, 2020
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:
Page last updated:





