Patient-centred care for healthcare providers
Key points about patient-centred care
- Patient-centred care can be defined as "providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions." (Institute of Medicine)
- Find information on the principles of patient-centred care and resources for additional learning.

The widely accepted dimensions of patient-centred care are:
- respect
- emotional support
- physical comfort
- information and communication
- continuity and transition
- care coordination
- involvement of family and carers
- access to care.
These dimensions form the backbone of numerous quality improvement programmes and surveys measuring patients’ experience of health care.
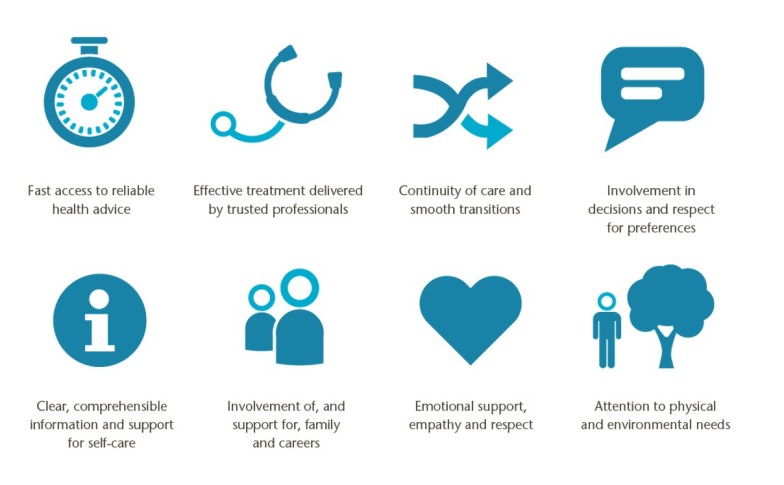
(Image source: Picker Institute, Europe)
There is now clear research demonstrating that patient-centred care improves patient care experience and creates public value for services. (1)
"When healthcare administrators, providers, patients and families work in partnership, the quality and safety of health care rise, costs decrease, and provider satisfaction increases and patient care experience improves. Patient-centred care can also positively affect business metrics such as finances, quality, safety, satisfaction and market share." (1)
World Health Organisation, May 2015
Patient-centred care has been increasingly recognised as a critical dimension of high-quality health care since the landmark Institute of Medicine report, Crossing the Quality Chasm (2) included it as one of the six quality aims for improving care. These aims are built around the core need for health care to be:
- Safe: avoiding injuries to patients from the care that is intended to help them.
- Effective: providing services based on scientific knowledge to all who could benefit, and refraining from providing services to those not likely to benefit.
- Patient-centered: providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions.
- Timely: reducing waits and sometimes harmful delays for both those who receive and those who give care.
- Efficient: avoiding waste, including waste of equipment, supplies, ideas, and energy.
- Equitable: providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
In many countries, a patient-centred approach is now supported by national policies and Consumer Rights Charters. Within New Zealand, professional authorities such as the NZ Medical Council (NZMC) and the The Code of Health and Disability Consumers’ Rights uphold the importance of patient-centred care and a useful chapter in Cole's Guide to Good Medical Practice (NZMC) discusses the relationship between patient-centred care and cultural competence. (3)
The Health Quality and Safety Commission has a programme of work focused on Partners in Care(external link) and the new NZ Health Strategy(external link) has a related concept of people-powered as a core theme.
Internationally, in May 2016 at the Sixty-ninth World Health Assembly (WHA) Member States adopted, with overwhelming support, resolution WHA 69.24 “Strengthening integrated people-centred health services”(external link) that supports the “Framework on integrated people-centred health services”. (4)
Delivering person centred care in long-term conditions
Transforming support for people with long term conditions makes sense from every angle: improving wellbeing, developing a more positive sense of control, achieving better health outcomes, and potentially lower healthcare costs. It now seems possible to envisage this as the norm but substantial barriers and challenges exist. We need clinical and patient leadership to help navigate these challenges, along with system drivers and incentives, and practical support to encourage these new ways of working. People with lower activation levels, poor health literacy, and difficult social circumstances need specific and tailored support but have the most to gain.11 We believe that the success of any clinician, team, or organisation should be defined by their efforts to tackle these disadvantages and to ensure a person’s goals and priorities are always at the centre of his or her care.
Read more about the article here.(external link)
Patient commentary: What I need to self manage my care
Alex, a 27 year old with type 1 since age 18 months talks about what's helped her and what's needed for patient-centred care.
What helps:
- Medical devices and repeat prescriptions
- Multidisciplinary healthcare team in secondary care
- Education
- Empathy
- Engagement
- Integrated services
"For me the next logical steps are to create my own care plan, containing goals set and measured by me and accessible at a time and location that suits me (online or offline), and to work with the stakeholders I choose, from the list mentioned above, so that I can achieve and update my care plan."
What doesn't help:
"What I don’t want is to be given routine outpatient appointments. People don’t want to spend time in clinics to manage their health; they want to do it at home in a way that suits them, like their banking or shopping. This is person-centered care and in some places it’s already happening."
What's needed:
But we will only get universal person-centered care when we begin valuing, measuring, and responding to the things that patients really care about – and doing so in a systematic, fully integrated 'whole system' way." (1)
Read the full BMJ article(external link).
Patients as partners – a guide
Building collaborative relationships among professionals, patients, carers and communities.
Key messages
The guide suggests five approaches to developing an effective relationship:
-
- find your collaborative partner: this, together with identifying funding and a real task to work on, marks the first important stage of beginning a collaborative relationship
- invest in developing leadership and collaborative relationships
- make time for learning: set aside time for reflection, record learning and share that learning with peers and those you hope to influence
- go where the energy is: sometimes this means working under the radar for a while until you are ready to share your results, your approach and your learning
- embed collaborative activity at all levels in your system or organisation.
Source: The Kings Fund – ideas that change healthcare, UK
Patient–centered care: the key to cultural competence
This article summarises the key principles of patient–centered cultural competence and relevant skills, phrases and examples.
Read full article here(external link).
Source: Annals of Oncology, Oxford Academic.
Ten commandments for patient-centred treatment
Lehman, R. Tejani, A. et al. Ten Commandments for patient-centred treatment.(external link) Br J Gen Pract Oct 2015, 65 (639) 532-533
References
- Silverstein A. Patient commentary: What I need to self-manage my care(external link) BMJ 2015; 350 :h248
- Lehman, R. Tejani, A. et al. Ten Commandments for patient-centred treatment.(external link) Br J Gen Pract Oct 2015, 65 (639) 532-533
Videos about patient centred care, ranging from discussions about the future of patient-centred care (at TEDx University of Minnesota), to a study showing that person-centred and community-centred approaches for health and wellbeing are pivotal to improving health and wellbeing outcomes.
Patient-centred care – the future
Dave Moen talks about the future of patient-centred care (at TEDx University of Minnesota).
(TEDx Talks, 2012)
David Moen, M.D., is an emergency department physician and led the development of Fairview Health Network—an integrated, multi-specialty provider network built on the belief that providers are in the best position to transform care. (speaks at TEDxUMN University of Minnesota in August 2012, 21.56 mins)
Practical learning tips to put people and communities at the heart of health and wellbeing
"The Realising the Value programme conducted analysis of the evidence for person-centred and community-centred approaches for health and wellbeing, working with five frontline sites across England, and published tools, recommendations and economic modelling to show how they can be successfully implemented. It concluded that that person and community-centred approaches are pivotal to improving health and wellbeing outcomes."
(The Health Foundation, UK)
New Zealand
- Partners in care(external link) Programme of work by the Health Quality and Safety Commission
- Cole’s medical practice in New Zealand,(external link) 12th edition. Medical Council of New Zealand
- The Code of Rights(external link) Health & Disability Commissioner
- New Zealand Health Strategy 2016(external link) Ministry of Health, NZ
- Code of Conduct(external link) Nursing Council of New Zealand
- The path to patient centred care in New Zealand’s health system June 2016(external link) Association of Salaried Medical Specialists
- Centre for Person-Centred Research(external link) Auckland University of Technology (AUT)
-
Realising the value [PDF, 3.9 MB] 2016 Ten key actions to put people and communities at the heart of health and wellbeing
International
- Crossing the Quality Chasm: A New Health System for the 21st Century, 2011(external link) Institute of Medicine
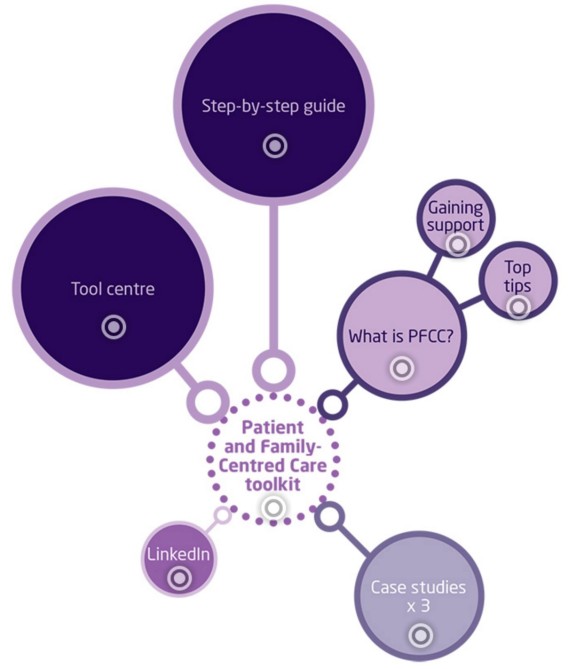
- Patient and Family-Centred Care toolkit(external link) The Point of Care Foundation UK
- Framework on people-centred integrated health services 2016(external link) World Health Organisation
- Person-Centred Care Resource Centre(external link) Health Foundation, UK
- Research, strategy, measurement and more for person-centred care(external link) Picker Institute Europe
- Patient-Centered Primary Care Collaborative(external link) USA
- Principles of patient-centered care(external link) Picker Institute, USA
Realising the Value (Health Foundation UK) – resources
"The Realising the Value programme conducted analysis of the evidence for person-centred and community-centred approaches for health and wellbeing, working with five frontline sites across England, and published tools, recommendations and economic modelling to show how they can be successfully implemented. It concluded that that person- and community- centred approaches are pivotal to improving health and wellbeing outcomes."
|
Realising the Value – Resources |
|
Realising the value [PDF, 3.9 MB] 2016 |
|
What the system can do [PDF, 1.6 MB] 2016 |
|
Making it happen [PDF, 9.2 MB] 2016 |
|
Spreading change [PDF, 1.6 MB] 2016 |
|
Supporting self-management [PDF, 706 KB] 2016 |
|
Making the change(external link) 2016 |
|
At the heart of health [PDF, 910 KB] 2016 |
|
How should we think about value in healthcare?(external link) 2015 |
- Australian Commission on Safety and Quality in Healthcare. Improving quality (external link)and safety through partnerships with patients and consumers. Discussion paper 2011
- Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century, 2011(external link)
- Morris, K 2017. Cultural competence and patient centred care Chapter 17(external link) in St George IM (ed.). Cole’s medical practice in New Zealand, 13th edition. Medical Council of New Zealand, Wellington
- Framework on people-centred integrated health services 2016(external link) World Health Organisation
- People-centred and integrated health services: an overview of the evidence,(external link) May 2015, World Health Organisation
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Page last updated: