If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Mpox
Advice for cases linked to the Clade II outbreak
Key points about mpox
- Mpox is a viral infection that causes a rash and possible flu-like symptoms.
- It's spread through direct physical contact with the sores or lesions of someone with mpox.
- You can spread mpox to others until all your sores are healed.
- If you have mpox you won't need to isolate. Your healthcare provider will advise you on what to do to prevent spreading mpox to others.
- This page provides more information about mpox and what to do if you have it or have been in contact with somebody who has. Note that the advice applies to cases linked to the current global Clade II outbreak.

There has been an increase in locally acquired mpox cases in Aotearoa New Zealand, almost 20 cases have been reported since July 2025. Aotearoa New Zealand is at risk of mpox from people returning from overseas due to the ongoing global outbreak of Clade II mpox.
Mpox (formerly known as monkeypox) is a viral disease. There are different types (called clades) of mpox and the advice on this page applies to Clade II mpox only.
Most people recover fully without treatment but in some cases, people can get seriously ill.
Since May 2022, there has been a global increase in mpox cases reported from multiple countries where it's not usually seen. See the 2022–2023 mpox outbreak global map.(external link) Note that this map is no longer being updated.
In Aotearoa New Zealand, mpox is a notifiable disease which means it must be reported to Public Health Services. Reporting an infection of mpox helps to control and contain the spread throughout the motu (country).
People at highest risk are those who have close physical, intimate or sexual contact with a confirmed mpox case. Globally, mpox has mostly affected:
- men who have sex with men (MSM)
- people who have sex with MSM – this may include people of any gender or sexual identity, whether they are transgender or cisgender, and non-binary people.
Symptoms usually appear 1 to 3 weeks after you've been exposed to the virus. The first symptoms of mpox are often flu-like symptoms including:
- headache
- fever (temperature higher than 38°C)
- chills
- muscle aches
- backache
- swollen lymph nodes in your neck, armpits or groin (this is a symptom that differs from chickenpox)
- tiredness.
Most people will then get spots, bumps, blisters or sores appearing on their skin after a few days. These are known as lesions. Lesions can affect any part of your body including you face and mouth, arms and legs, genitals and anus.
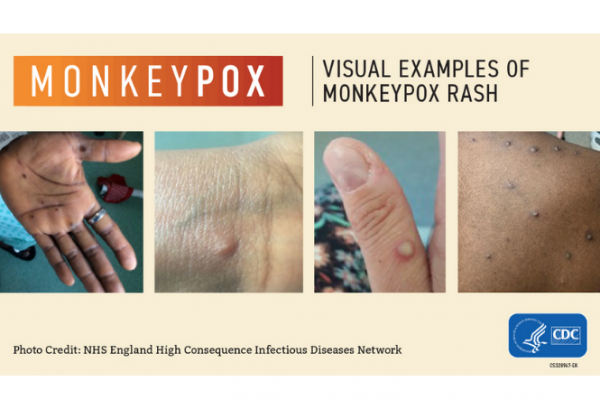 Image credit: NHS England High Consequence Infectious Diseases Network
Image credit: NHS England High Consequence Infectious Diseases Network
It’s possible to have lesions without other symptoms. The number of lesions varies from one or a few to many.
The lesions change by going through different stages, as chickenpox does. They start off flat then become raised and filled with fluid before crusting over and finally forming a scab that falls off. Mpox is diagnosed by swabbing these skin lesions for the virus.
The lesions are often painful and itchy. Your healthcare provider can give you some pain medicine to help with this.
You may also have pain, bleeding or an uncomfortable feeling in your nono or bum (anus).
The symptoms usually go away by themselves within 2 to 4 weeks. It’s usually a mild illness, but a small number of people become very unwell.
Mpox isn’t easily spread between people. The risk of the virus spreading widely in Aotearoa New Zealand is very low. It’s caught from:
- direct contact with the skin lesions, scabs, or body fluids (such as pus or blood) and possibly through semen – it's most commonly spread through sexual or intimate contact
- touching clothing, bedding towels or other objects which have been used by the person with mpox
- pregnant people spreading the virus to their foetus (unborn baby) through the placenta.
There’s a small risk of getting mpox from breathing in the same air that somebody with the virus has just breathed out, but there needs to be long and close contact for this to happen.
Mpox can spread (is contagious) as soon as symptoms start until the rash has fully healed and a fresh layer of skin has formed. The infection generally lasts 2 to 4 weeks.
If you are a close contact of someone with mpox you should monitor for symptoms for 21 days from when you last had contact with them. You should also avoid sexual or intimate contact with others for this time period.
If you develop any symptoms within 21 days, contact your healthcare provider for further advice.
If you think you may have been in contact with someone who has mpox, get advice from your healthcare provider. They will ask you about your symptoms, how and when you were in contact with people who may have mpox and any recent travel.
Many illnesses can cause similar symptoms, so you are unlikely to have mpox if you're not in a high-risk group. It is still important to check with a healthcare provider.
Mpox is not very infectious. To get infected you generally need to have had contact with the lesions of a person with mpox.
If you're at risk of mpox and you develop symptoms, please seek medical help. You can contact your local sexual health clinic for free advice, call your GP or ring Healthline on 0800 611 116.
- If you test positive for mpox, public health staff will be in contact to support you and provide advice on your symptoms and the precautionary measures you need to take to prevent spreading mpox to other people. You will not be asked to isolate.
- For some people with mpox, the skin lesions or sores can become itchy or painful. Your healthcare provider can prescribe pain relief if you need it.
- Occasionally people with mpox can become very sick. If your symptoms are getting worse, contact your healthcare provider for advice.
- If you need to attend a healthcare setting, advise them you have mpox. Cover any lesions or sores and wear a mask during your visit.
- If you're feeling seriously unwell and require the support of emergency services, call an ambulance on 111 and let them know you have mpox.
Stopping the spread
Because the virus is spread though close contact with an infected person and their bedding, clothing and personal things it’s important to practice good hygiene to reduce the risk of spreading mpox to other people.
This includes:
- keeping scabs and lesions covered until the skin has healed which can take 14 to 28 days
- avoiding physical contact with others, including sharing a bed, kissing, intimate touching
- not sharing clothing, bedding or utensils
- cleaning the bathroom after use
- avoiding contact with pregnant people, young children, people with severe eczema and immunocompromised people
- avoiding contact with household pets as they can get and spread the virus.
Read more about how to avoid spreading mpox(external link).
Treatment involves managing the symptoms so make sure you:
- Drink plenty of fluid so you stay well hydrated.
- Eat well.
- Get plenty of rest.
- Take pain medicine (paracetamol) if needed for pain and fever and talk to your healthcare provider if you need something stronger.
- Keep any lesions clean by washing your skin gently with soap and warm water to reduce the risk of infection.
- Take an antihistamine if the lesions are itchy.
- Watch out for any signs of an infected lesion – it may get red, sore, swollen, shiny and hot. Seek advice from your healthcare provider if this happens.
Returning to normal activities
Your healthcare provider will monitor you and advise when you can return to normal activities.
The virus may be present in semen for up to 3 months after your symptoms have resolved. It’s recommended you use condoms during sexual activity where semen could come into contact with another person. For more information contact a sexual health clinic(external link).
Limiting risks
Avoid close contact with people with suspected or confirmed mpox and don't share their clothing, bedding and utensils.
Make sure you feel well and have no mpox symptoms before having close physical or sexual skin-to-skin contact with others.
Vaccination
The mpox vaccine called Jynneous® has been given provisional approval by Medsafe for eligible people. If you’re at higher risk of getting mpox, talk to your healthcare provider about being vaccinated.
The vaccine is currently free (though consultation fees may apply) and available to:
- Gay, bisexual and other men who have sex with men (MSM).
- people who have sex with MSM. This may include people of any gender or sexual identity, whether they are transgender, cisgender or non-binary people.
- Anyone who is a close contact of someone who has been infected with mpox.
Find out more about how to book a mpox vaccine.(external link)
Mpox(external link) Health New Zealand | Te Whatu Ora
Mpox – what you need to know(external link) World Health Organization
Brochure
Mpox(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
Mpox poster [JPG, 81 KB] Health New Zealand | Te Whatu Ora, NZ, 2024
References
- Mpox (te koroputa maki)(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
- Mpox(external link) World Health Organisation, 2022
- Mpox(external link) Health New Zealand | Te Whatu Ora
- Mpox(external link) Auckland Sexual Health Service, NZ, 2022
- Mpox vaccines(external link) Burnett Foundation, NZ, 2024
Mpox(external link) Health New Zealand | Te Whatu Ora
Mpox clinical guidance(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
Clinical features of Mpox(external link) CDC, US, 2024
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Sharon Sime, Public Health Physician | Medical Officer of Health, Health New Zealand | Te Whatu Ora
Last reviewed:
Page last updated:





