Rituximab is used to treat certain types of cancers such as non-Hodgkin's lymphoma and chronic lymphocytic leukemia. It is also used as an anti-rejection treatment for solid organ transplants.
Rituximab is also used to treat rheumatoid arthritis. It is used with methotrexate to treat moderate-to-severe forms of rheumatoid arthritis, usually only after other medicines have not worked. It can reduce inflammation, pain, swelling and joint damage.
Rituximab belongs to a group of medicines known as biologic medicines. These are medicines that target specific chemicals in your body involved in the inflammatory response that causes rheumatoid arthritis. Other examples of biologic medicines used for rheumatoid arthritis are tocilizumab and tumour necrosis factor (TNF) inhibitors (such as Humira, Enbrel and infliximab). The dose of rituximab depends on the condition it is being used for.
Rituximab
Sounds like 'rye-TUX-ih-mab'
Key points about rituximab
- Rituximab is also used to treat rheumatoid arthritis and some types of cancers.
- Rituximab is also called Mabthera or Riximyo.
- Find out how to have it safely and possible side effects.

Rituximab is given in hospital by slow injection into a vein in your arm (called intravenous infusion). The infusion usually takes 2–4 hours. For rheumatoid arthritis, the course of treatment is 2 infusions given 2 weeks apart. The infusion may be repeated when the improvement is wearing off, or to stop a flare-up of your arthritis. This can be anything from 6 months to a few years later. Many people need to have rituximab infusions at least once a year.
During the infusion
Rituximab can cause a reaction while it is being infused. This usually happens within 30 minutes to 2 hours after starting the first infusion. You may have trouble breathing, or experience fever, chills, flushing, skin rash, itching, dizziness or headache. Tell the nurse immediately if any of these symptoms occur. This reaction is usually mild and can be controlled by giving rituximab more slowly. You will also be given medicines, such as paracetamol and an antihistamine, shortly before the infusion to help control this reaction. Once the symptoms have gone away the speed of the infusion can usually be increased again.
Like all medicines, rituximab can cause side effects, although not everyone gets them. Often side effects improve as your body adjusts to the new medicine.
Increased risk of infections
Because rituximab can weaken your body's immune system, it can make it more likely for you to get infections. These infections may be mild (such as colds or sinusitis) or more severe such as TB (tuberculosis) and septicaemia (infection of your blood).
- Before starting rituximab you need to:
- have blood tests and a chest x-ray to check for infections and to check your liver
- check with your doctor what vaccines you might need – you should not have a live vaccine while using rituximab.
- Tell your doctor immediately if you:
- come into contact with someone who has an infection such as TB (tuberculosis) while you are taking rituximab
- develop an ongoing cough, weight loss, fever, sore throat, bruising or bleeding.
- You will need to be monitored for infections during treatment and for several months after you have stopped taking it.
- Before you start taking rituximab let your doctor know if you are pregnant or planning to become pregnant or if you have TB or hepatitis B.
| Side effects | What should I do? |
|---|---|
|
|
|
|
|
|
|
|
| Read more about medicines and side effects and reporting a reaction you think might be a side effect. | |
Rituximab(external link) RheumInfo
Mabthera(external link) Consumer Information Sheets, Medsafe, NZ
Rituximab(external link) Australian Rheumatology Association
References
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
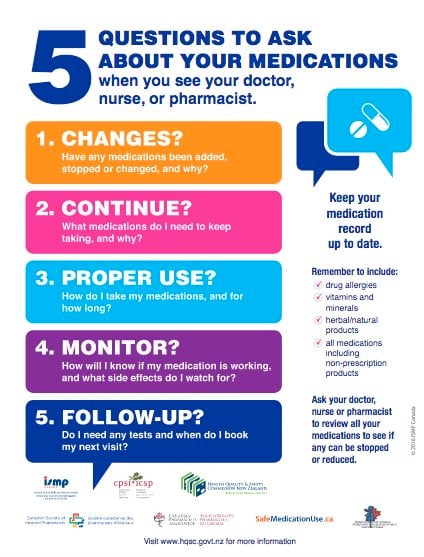
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Maya Patel, MPharm PGDipClinPharm, Auckland
Last reviewed:
Page last updated:





