Ticagrelor is an anti-platelet medication. It is usually used in people who have symptoms of chest pain (angina) or who have had a heart attack (myocardial infarction) to reduce the risk of having a further heart attack or stroke. It blocks certain blood cells called platelets and slows down your body’s ability to clot blood. It is used to prevent blood clots forming in blood vessels that lead to your brain and heart muscle. Preventing blood clots in these vessels helps lower your risk of stroke and heart attack.
We're aware of a problem when trying to use Zero Data to link to Healthify. Zero Data is managed by Health NZ and we are working with them to get this fixed.
Ticagrelor
Sounds like ('tie-kag-re-lore')
Key points about ticagrelor
- Ticagrelor is an antiplatelet medicine, which means it makes it less likely your blood will clot.
- Ticagrelor is also called Brilinta®.
- Find out how to take it safely and possible side effects.

In New Zealand ticagrelor is available as tablets (90 mg).
- The usual dose of ticagrelor is 90 mg (1 tablet) two times a day. You may be given a starting dose of 2 tablets the first time you take it.
- Ticagrelor is usually taken together with low-dose aspirin for up to 12 months.
- Always take your ticagrelor exactly as your doctor has told you. The pharmacy label will tell you how much ticagrelor to take, how often to take it and any special instructions.
- Timing: Take your ticagrelor doses at the same times each day, in the morning and the evening. You can take ticagrelor with or without food.
- Swallow your tablets with a glass of water. If you have problems swallowing the tablet, you can crush it and mix it with half a glass of water, just before taking it. To make sure that there is no medicine left, rinse the empty glass with another half a glass of water and drink it.
- Missed dose: If you forget to take your dose, take it as soon as you remember that day. But, if it is nearly time for your next dose, just take the next dose at the right time. Do not take double the dose.
- Tell your healthcare provider: It is important to let anyone who gives you treatment know that you are taking ticagrelor, including your dentist, pharmacist, podiatrist and nurse. You may need to stop using this medicine for several days before having surgery, dental appointments or medical tests.
Like all medicines, ticagrelor can cause side effects, although not everyone gets them. Common side effects include nausea (feeling sick), shortness of breath, feeling dizzy or light headed and diarrhoea (runny poos). These usually go away with time. Tell your doctor if troublesome.
Increased risk of gout
Ticagrelor can increase the level of uric acid in your blood and cause a flare up of gout. Tell your doctor if you get severe pain and swelling in your joints – these are signs of gout.
Increased risk of bleeding
Ticagrelor increases your risk of bleeding. You might bleed or bruise more easily while you are taking ticagrelor. Minor bleeding such as a nosebleed should usually stop on its own. If you have a fall or hurt your head or body, get medical attention immediately, even if you feel okay.
Signs of severe bleeding
If you have any of the following signs of bleeding, contact your doctor immediately or ring Healthline for free 24-hour health advice 0800 611 116:
- becoming pale, very weak and tired, or short of breath
- any bleeding from your gums or cuts or nosebleeds that won’t stop
- blood in your stools (poo) – black, tarry stools
- blood in your urine (wee) – pink, red or brown-coloured urine
- coughing up blood or vomit that looks like coffee grounds
- sudden numbness or weakness of your arm, leg or face, especially if only on one side of your body
- sudden confusion, difficulty speaking or understanding others
- sudden difficulty in walking or loss of balance or co-ordination
- suddenly feeling dizzy or sudden severe headache with no known cause.
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
Ticagrelor should not be taken with some other medications and herbal supplements, so always check with your doctor or pharmacist before starting ticagrelor or before starting any new medicines. Also check with your pharmacist before taking:
- over-the-counter anti-inflammatories such as diclofenac (eg, Voltaren Rapid), ibuprofen (eg, Nurofen), naproxen (eg, Naprogesic)
- herbal extracts such as garlic, ginkgo or ginseng.
Taking these together with ticagrelor may increase your risk of bleeding and should be avoided.
The following links provide further information on ticagrelor.
Ticagrelor(external link) New Zealand Formulary Patient Information
Brilinta®(external link) Medsafe Consumer Information Sheet (NZ)
Resources
Ticagrelor in te reo Māori(external link)(external link) My Medicines, NZ, 2017
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- Ticagrelor – out with the old, in with the new?(external link) BPAC, NZ, 2013
- An update on antithrombotic medicines - what does primary care need to know?(external link) BPAC, NZ, 2015
- Ticagrelor(external link) New Zealand Formulary
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
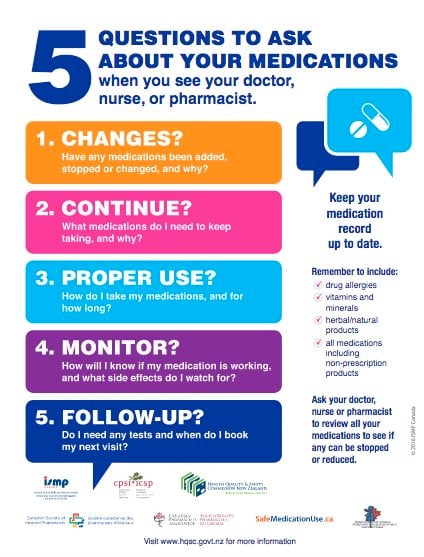
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





