If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Mirena for menopausal hormonal treatment
Key points about Mirena for menopausal hormonal treatment
- Mirena® is an intrauterine device (IUD) that contains progestogen.
- It may be used together with oestrogen as menopausal hormone therapy for people who still have a uterus (womb).
- Find out about Mirena for menopausal hormonal treatment.

Mirena® is an intrauterine device (IUD) that contains progestogen. It may be used as menopausal hormone therapy (MHT) in combination with oestrogen for people who still have a uterus (womb).
- Mirena is a small, white T-shaped plastic device with a stem attached to 2 removal threads that is placed inside your womb (uterus).
- It slowly releases a small amount of the hormone progestogen (as levonorgestrel) directly into your uterus, so hardly any goes into the rest of your body. Because of that, many women have fewer whole-body side effects compared to other progestogen preparations.
- Once it's put in, Mirena lasts for up to 5 years when you're using it as part of your MHT. See below for how long you can have the Mirena in for MHT.
- It can be put in at your GP clinic and you generally don’t need an operation or a general anaesthetic for this.
Why is a progestogen needed with oestrogen, in people who have a uterus?
- If you still have your uterus, your MHT will include both oestrogen and progestogen because oestrogen alone can overstimulate the cells lining your uterus, causing an increased risk of cancer of the uterus lining.
- The progestogen in Mirena helps to prevent the thickening of the lining and therefore reduces the risk of cancer.
- Some people will take progestogen tablets or capsules by mouth and others will have a Mirena which delivers the progestogen directly to the womb lining and keeps it thin.
Mirena also eases heavy or painful periods and it can reduce menstrual flow and, for some, stop periods completely, which is often a huge relief during perimenopause. In addition, it provides effective contraception and is one of the most reliable birth control methods available. It's not affected by other medicines.
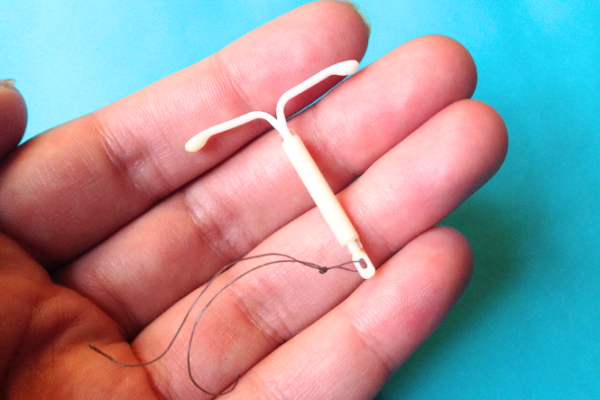
Image credit: Sarahmirk via Wikimedia Commons(external link)
Before the IUD is put in, you'll need to have a pelvic examination. The healthcare provider will check the size and position of your womb (uterus).
The IUD is then put in using a small plastic introducer.
- Putting in an IUD can sometimes be uncomfortable. Read more about discomfort or pain during the fitting of an IUD.
- Light vaginal bleeding may also occur for a short while afterwards. Use pads rather than tampons or menstrual cups for the first few days after your IUD is put in.
- It’s also recommended to avoid sex, swimming and baths for the first few days after a Mirena is put in.
- Your healthcare provider will usually want to check that there are no problems a few weeks after an IUD is put in. This is best done after your next period. After this, there's no need for any routine check until it's time to remove the IUD. However, contact your healthcare provider at any time if you have any problems or queries.
Checking the IUD is in place
- Rarely, the IUD can come out. The risk is higher if you have a high body mass index (BMI).
- If the IUD comes out, it's no longer effective. You may be able to have a new IUD fitted.
- You’ll be taught how to feel for the threads of the IUD so you can check it’s in place. It’s best to check the threads monthly, after each period or at the beginning of each month.
- If you can’t feel the threads, it may not mean that the IUD has fallen out. Sometimes the threads are difficult to feel or have been pulled up into the cervical canal (which won’t harm you).
- Contact your healthcare provider if you can’t feel the IUD threads.
Removal of Mirena
The IUD can be taken out at any time if you’d like it removed. This needs to be done by a trained healthcare provider.
Risk of blood clots
- The risk of blood clots in the legs, arms or the lung increases with increasing age, increased body weight, smoking, and with illnesses including cancer and some autoimmune diseases.
- Mirena itself does not increase the risk of deep vein thrombosis (DVT). However, when it’s used as part of MHT, it’s combined with oestrogen. Oestrogen patches and gels carry little to no risk of blood clots, whereas oestrogen tablets slightly increase the risk (1 extra blood clot per 1,000 women).
If you're worried about the risk of blood clots, talk to your healthcare provider.
Any pain or discomfort you feel during and after an IUD is put in or removed is different for everyone. If you’re worried about pain or discomfort it’s a good idea to talk to your healthcare provider before you have it fitted to discuss your options. You can take a support person with you when you have your IUD put in and removed.
When the IUD is put in
- Most people feel some discomfort or pain. The type of IUD (hormonal or copper), your pain tolerance, and whether you’ve given birth before can influence how painful it feels.
- The pain might feel like cramping or a sharp pinch that lasts for a few minutes. Some compare it to a strong period cramp.
- To help reduce pain during the procedure, your healthcare provider may suggest taking over-the-counter pain relievers such as paracetamol and ibuprofen about 1 hour before the procedure.
- It’s important to tell your healthcare provider if you’re having pain during the procedure.
Video: IUD insertion and pain – what to expect with Dr McNamee
(Sexual Health Victoria, Australia, 2023)
After the IUD is put in
- It's common to experience cramping after the IUD has been put in. For some people the cramps may be mild and go away within a few hours. Others may have stronger period-like cramps for a few days afterwards.
- The cramps can vary, but they usually lessen over time. You can use pain relievers such as paracetamol and ibuprofen. A hot water bottle or heat pad may also help.
If you have a sudden and severe attack of pain or any continuous lower abdominal pain, you should seek medical advice.
During removal of the IUD
- The pain level when removing an IUD can vary from person to person, but it's generally minimal. Some people get mild discomfort while rarely others might feel stronger pain.
- The removal process usually only takes a few minutes, and while it may feel uncomfortable, it's generally quick.
- Some people may be advised to take pain relief before the removal of the IUD to help with pain and discomfort. If the IUD is difficult to remove, it can be more uncomfortable.
Every person is different and the length of time you'll have menopausal symptoms for is unknown. When you first start MHT, it’s important to have regular check-ups with your healthcare provider to assess whether ongoing MHT is right for you. However, once you are settled on a suitable dose for you, you'll need less frequent check-ups (once every year).
You'll need to have progestogen for as long as you're using oestrogen
- Mirena works for a maximum of 5 years as the progestogen component of MHT. Most people have no problems, and the IUD can remain in place for that time.
- You can keep it for 8 years for contraception or heavy periods but would need to start taking progesterone capsules (Utrogestan) after 5 years as the progestogen component of your MHT.
- At the end of this time, you'll need to visit your healthcare provider to see if your Mirena needs to be replaced with a new one.
Why is Mirena recommended to be replaced after 5 years when used in MHT, but can be effective for up to 8 years when used for contraception or heavy periods?
When Mirena is used as part of MHT, its job is to protect the lining of the uterus from the oestrogen you’re taking. To do this, the Mirena must release enough hormone every day to keep the lining thin and healthy. After 5 years, the amount of hormone it releases drops too low to reliably protect the womb lining. So, it’s safe and effective for 5 years in MHT, and then it should be replaced or supported with extra progestogen (eg, Utrogestan capsules).
When used for contraception or heavy periods, Mirena is effective for up to 8 years. That’s because when used for birth control or to treat heavy periods, Mirena doesn’t need to release quite as much hormone to work. Studies have shown it still works very well for up to 8 years, when used to prevent pregnancy and reduce bleeding.
Like all medicines, Mirena can cause side effects, although not everyone gets them. If you're concerned about any symptoms you think might be related to it, talk to your healthcare provider. The following information offers some guidance but doesn't include all possible side effects.
Common side effects
Most women will have daily light bleeding or some spotting for up to six months after insertion of a Mirena. This is completely normal and is nearly always much lighter than a period.
Tell your healthcare provider immediately or phone Healthline free on 0800 611 116 if these occur
- Signs of infection such as severe pain in your lower tummy area, fever, flu-like symptoms, feeling unwell, dizziness, feeling faint, pain during sex or vaginal discharge.
- Depression or nervousness.
- Migraine or severe headaches.
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
Combined Menopausal Hormone Therapy (MHT)(external link) Australasian Menopause Society
Brochures
Mirena – your questions answered(external link) Bayer New Zealand Limited, 2022
Medicines and side effects [PDF, 91 KB] Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- Mirena(external link) Medsafe datasheet, NZ
- Mirena(external link) Medsafe Consumer Information Sheet, NZ
- van Hylckama Vlieg A, Helmerhorst F, Rosendaal F. The risk of deep venous thrombosis associated with injectable depot-medroxyprogesterone acetate contraceptives or a levonorgestrel intrauterine device(external link) Arterioscler Thromb Vasc Biol. 2010;30(11):2297-300.
Brochures

Bayer New Zealand Limited, 2022
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

5 questions to ask about your medications
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Alison Payne, Specialist General Practitioner, Martinborough
Last reviewed:





