You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Medicines and tendon problems
Key points about medicines and tendon problems
- For some people, some medicines can cause problems with their tendons, such as pain, swelling and reduced movement.
- Although the Achilles tendon is most commonly affected, other tendons may also be affected such as those in your hands or wrists.
- Find out more about medicines and tendon problems.

Tendons are bands of strong connective tissue that attach muscle to bone. For some people, some medicines can cause problems with their tendons. Read more below about examples of medicines that can cause tendon problems.
Medicines may cause tendinitis, where the tendon's become inflamed, leading to symptoms such as pain, swelling and reduced movement. Read more about tendinitis.
Although the Achilles tendon (at the back of your leg above your ankle) is most commonly affected, it can occur in any tendon including tendons in your shoulder, elbow, wrist, hand or knee.
Risk factors for medicine-related tendon problems
Some people are at increased risk of medicine-related tendon problems, for example:
- older adults, because of age-related changes and becoming less active
- people who are obese
- people who increase physical activity too quickly, because of high loads or heavy weights they're not used to, or sudden twists or stress on the muscle and tendon
- people who already have autoimmune connective tissue conditions or kidney failure
- people taking 2 or more medicines known to induce tendinopathy.
If you think that a medicine you take is causing tendon problems, talk with your doctor, pharmacist or physiotherapist.
Not all tendon problems are caused by medicines, so working out if your symptoms are caused by your medicine is not always easy. If you have noticed pain, swelling and reduced movement in your joint or joints, when you started a new medicine or when you increased the dose of a medicine you were already taking, it could be because of your medicine. However, sometimes it can take several weeks or months for these effects to occur.
If you're taking a medicine and you're worried that it might be affecting your tendons don't stop taking your medicine suddenly. Instead discuss this with your doctor, pharmacist or physiotherapist.
Sometimes there might be a different medicine you can take that has less effect on your tendons. Also, the risks of stopping or changing medicines should be balanced against the risks of tendon problems and other health effects.
The following are examples of medicines most commonly associated with tendon problems.
Note: This isn't a complete list. If you are unsure if the medicine you are taking can cause tendon problems, ask your doctor, pharmacist or physiotherapist.
Quinolone antibiotics (ciprofloxacin, levofloxacin, moxifloxacin, norfloxacin)
- Tendon problems can happen within 48 hours of starting the medicine or up to several months after stopping treatment.
- The Achilles tendon is most commonly affected.
Steroids when taken long term
- Some people are prescribed steroid medicines on an ongoing basis for the treatment of long-term conditions.
- Taking steroids long term is helpful to treat conditions associated with inflammation, but ongoing steroid use can cause side effects.
- People taking steroids for longer than 3 months, for autoimmune connective tissue disorders such as rheumatoid arthritis and systemic lupus erythematosus are particularly at risk.
Statins (atorvastatin, pravastatin, rosuvastatin, simvastatin)
- Tendon problems can occur at any dose and about 8 to 10 months after starting treatment.
Aromatase inhibitors (anastrozole, letrozole, exemestane)
- Tendons in the hands and wrists are most commonly affected.
- Tendon problems can happen from weeks to months of starting the medicine.
References
- Drug-induced tendinopathy(external link) Medsafe Presciber Update, NZ, September 2024
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
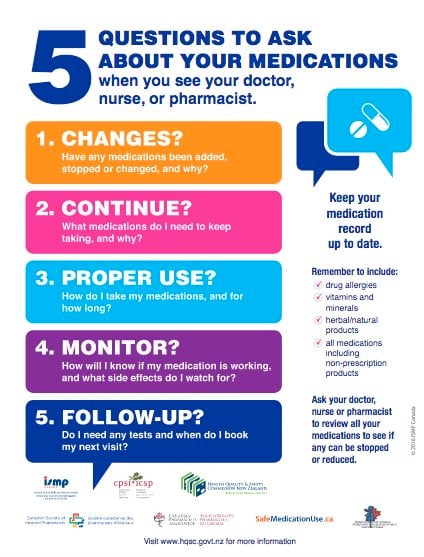
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland; Professor Gisela Sole, School of Physiotherapy, University of Otago
Last reviewed:





