| March 2023: The use of Evusheld as a COVID-19 prevention medicine is no longer recommended in Aotearoa New Zealand as it's not expected to work against most of the current COVID-19 variants. If you have recently received Evusheld as prevention and you have COVID-19 symptoms, you should do a test and seek early care if you think you may have COVID-19. |
Low or no data? Visit Zero Data then search for 'Healthify'. Click on our logo to return to our site and browse for free.
Evusheld
(Say ‘ev-YOU-sheld’)
Key points about Evusheld
- Evusheld contains 2 medicines – tixagevimab and cilgavimab.
- It is no longer recommended for COVID-19.
- Find out more about Evusheld, when it is used and possible side effects.

Evusheld contains 2 medicines – tixagevimab and cilgavimab. They belong to a group of medicines called monoclonal antibodies. They work by binding to the virus that causes COVID-19 infection (SARS-CoV-2) and preventing it from infecting healthy cells in your body.
The medicine is for people who have trouble making antibodies to fight disease, eg, if you have a weakened immune system (immunocompromised). Evusheld is best used before you get COVID-19. Your doctor will decide whether you need it or not. Read more about the access criteria for Evusheld.(external link)
Evusheld is not a vaccine, but consists of synthetic antibodies (made in the laboratory) which help to support your immune system to fight off infection.
Vaccines are different. They rely on your body to produce its own antibodies to prepare for being exposed to a particular virus. If you are exposed, your body will recognize it and know how to fight it off. For most people, vaccination is recommended as the best way to protect yourself against COVID-19.
Evusheld is given as 2 injections one after the other into a muscle (usually 1 injection into each of your buttocks). The injections will be administered by a doctor or nurse in a healthcare setting. Some people can have an allergic reaction to Evusheld, so you will be observed by the nurse or doctor for a short period after your injection.
Before you are given Evusheld, tell your healthcare provider if you have:
- low numbers of blood platelets (thrombocytopenia)
- had a heart attack or stroke, or other heart problems, or are at high-risk of cardiac (heart) events
- a bleeding disorder or are taking medicine to prevent blood clots
- any allergies to medicines
- any symptoms of COVID-19.
Sometimes a medicine isn’t suitable for a person with certain conditions or taking other medicines, or it can only be used with extra care. Your healthcare provider will give you more information about this.
If you are pregnant, breastfeeding or are planning to have a baby soon
There isn't a lot of research on the impact of Evusheld on pregnancy and breastfeeding. If you are pregnant, planning a pregnancy or breastfeeding, talk to your doctor about the potential risks and benefits.
If you have already had a COVID-19 vaccine
If you have received a COVID-19 vaccine, tell your healthcare provider before using Evusheld. It's possible that Evusheld may reduce your body’s immune response to a COVID-19 vaccine so you will need to have a gap of 2 weeks after your vaccination before receiving Evusheld.
As Evusheld is a new medicine, it's possible that we do not know all of the side effects yet.
Common side effects
These are usually mild and go away with time or when the medicine is stopped. Tell your healthcare provider if these side effects cause you problems or don’t go away.
- Pain, bruising of the skin, soreness, or swelling in the area where the injection was given.
Rare, serious side effects
Contact your healthcare team or Healthline on 0800 611 116 immediately if you notice these side effects and tell them you have had Evusheld.
- Signs of an allergic reaction such as:
- feeling short of breath, wheezing, difficulty breathing
- swelling of the face, lips, tongue, or other parts of the body
- severe itching of the skin, with a red rash or raised bump.
- Signs of blood clots or heart problems such as:
- pain, pressure, or discomfort in the chest, arms, neck, back, stomach, legs or jaw, abdominal pain
- shortness of breath
- swelling in your ankles or lower legs
- coughing up blood
- difficulties speaking or confusion
- loss of movement or weakness on one side of the body or face, severe headache.
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
References
- New Zealand’s COVID-19 treatments portfolio(external link) Pharmac, NZ
- Evusheld Consumer Medicine Information(external link) Therapeutics Goods Administration (TGA), Australia
- Frequently asked questions on the emergency use authorization for Evusheld (tixagevimab(external link)
co-packaged with cilgavimab) for pre-exposure prophylaxis (PrEP) of COVID-19(external link) FDA, US - COVID-19: Advice for all health professionals(external link) Health New Zealand | Te Whatu Ora
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
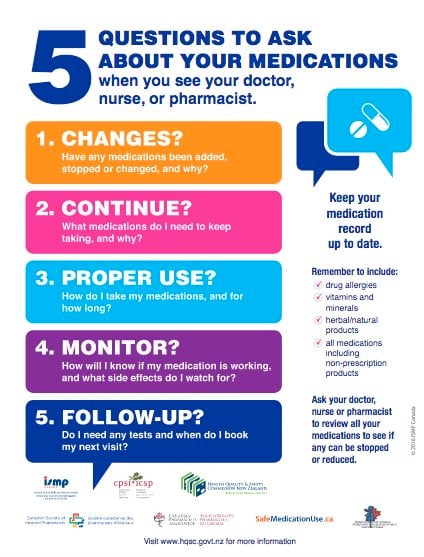
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





