Keratoconus is an eye condition that affects the front clear window of your eye (the cornea).
The shape of your cornea changes from its normal round shape to an irregular cone shape and this affects your vision. Your cornea gets thinner and your eye bulges out.
The cornea is the transparent front surface of your eye. If you have keratoconus, the cornea becomes thinned, distorted and irregular (cone shaped) and your eye bulges out. The shape of your cornea prevents the light entering your eye from being focused correctly on the retina at the back of your eye and distorts your vision.
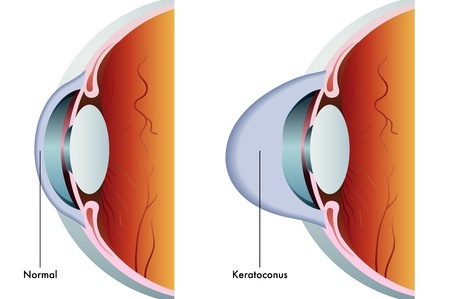 Image credit: 123rf
Image credit: 123rf
Keratoconus is usually seen in people who are very near-sighted and who have astigmatism. Though some can also be long sighted.
The changes and symptoms usually start in your early teens and can get worse in your 30s. It’s a progressive condition which can develop quickly, or can take many years to become apparent. It commonly affects both eyes, although sometimes only one eye is affected.






