Idiopathic pulmonary fibrosis (IPF) is a long-term condition that affects the lungs. In IPF, the lungs become thickened, scarred and stiff causing breathing problems.
- Idiopathic (means a condition where other known causes have been excluded).
- Pulmonary (relating to the lungs or respiratory system).
- Fibrosis (thickening and scarring of tissue).
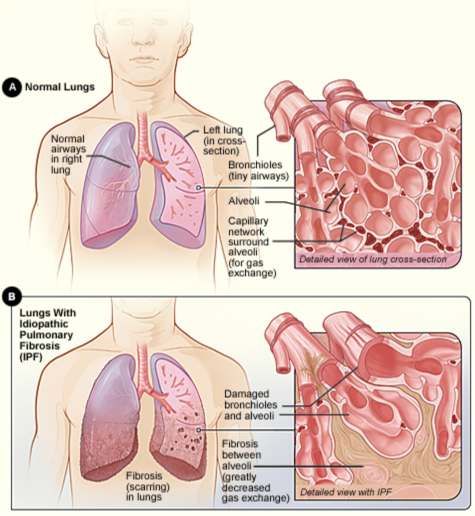
Image credit: NIH via Wikimedia Commons(external link)
The diagnosis can only be made after a full assessment and a number of investigations have been completed as requested by a respiratory specialist. Read more below and in the IPF diagnosis section.
As the scarring is progressive and irreversible, most people with IPF get worse over time. Each person experiences IPF differently. Some people can remain stable for many years, others get worse quickly. Medicines such as pirfenidone and nintedanib help to slow the rate of disease progression.
Things to know about IPF
- There’s no known cause for IPF. It's not an infection, a form of cancer or anything to do with COPD, cystic fibrosis or bronchiectasis.
- Signs of lung scarring on a chest X-ray or a CT scan are not enough to make a diagnosis of IPF. A full, comprehensive assessment is needed.
- Several lung conditions (eg, sarcoidosis, rheumatoid arthritis and scleroderma) may result in progressive lung scarring (fibrosis). But these conditions are treated differently.
- Several occupational lung diseases (eg, asbestosis or silicosis) and allergic lung conditions (eg, bird-fancier's lung) can also result in progressive pulmonary fibrosis. They too are treated quite differently and it's very important to have these ruled out before a formal diagnosis of IPF is made.
- IPF usually affects people over 60 years of age, and is rare in people under 50. Men are slightly more often affected than women.
- IPF is a serious and potentially fatal condition.










