If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Hymens and virginity
Does a broken hymen mean someone is not a virgin?
Key points about hymens and virginity
- Your hymen is a collar of tissue at the entrance to your vagina, with an unknown role.
- There's a lot of misinformation about it, as it's not commonly damaged by sexual activity or sports.
- Hymens change throughout life in response to hormone levels (primarily oestrogens).
- Virginity is a social and cultural concept, not a physical one. It doesn't have a biological basis, and it's about personal choice and how you define it. Virginity can't be 'taken away' or 'lost' as it's not a physical state.
- It's common not to bleed the first time you have sex – bleeding (or not) doesn’t say anything about virginity.
The hymen is a stretchy collar of tissue at the entrance to your vagina. It's protected by your labia. It can be compared to a scrunchie (hair tie) – with bunched-up tissue that expands when stretched (eg, during sex or using tampons) then returns to its bunched-up shape afterwards.
Hymens come in many different shapes and sizes. They may have a ring shape, half-moon shape or squiggly edges with notches – all of these are normal. The size of the opening in your hymen also varies in size and shape. There's no need to compare, or worry about whether your hymen fits a certain 'standard'. However, if you have any concerns about pain, discomfort or other issues, it's good to talk to a healthcare provider.
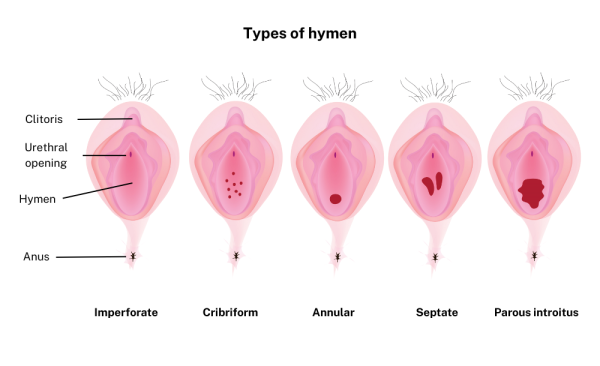
Image credit: Depositphotos
Hymens through history
Throughout history, patriarchal cultures have used the sexual history of girls and women to determine their status and value, as well as the status of their families and communities.
It's wrongly assumed that by looking at the hymen you can prove whether a woman is a virgin often based on the false belief that a ‘broken’ hymen proves sexual activity. Although this ‘virginity-testing’ has been condemned as a violation of human rights, it still continues in many parts of the world today and can be a controversial issue across different cultures and religions. These practices are not scientifically valid and can cause psychological harm. It's essential to understand that a person’s worth is not defined by their sexual history, and everyone has the right to their body autonomy and privacy.
Imperforate hymen is a medical condition where there's no opening (or a very small one) in your hymen. This becomes a problem with menstruation (periods) as blood cannot come out, causing pain. It may also cause problems with passing urine (peeing) or bowel motions (pooing).
You may also have difficulty with inserting tampons or having sex. This is an uncommon problem (about 1 in every 2000 females) and can require surgery under anaesthetic to give the hymen an opening to allow blood to flow. Less invasive treatments such as dilation may be considered for some people. It's important to talk to a healthcare provider to find out the best course of treatment based on individual needs.
Your hymen changes throughout your life.
- Before puberty, your hymen is thin and may be sensitive.
- During puberty, increased hormones (oestrogen) cause your hymen and other vaginal tissues to become thicker and more stretchy.
- During pregnancy, increased hormones cause your vaginal tissues to become even stretchier to allow for childbirth.
- Childbirth may also change the shape of your hymen and your vaginal tissues.
- With menopause and aging, your hymen and other vaginal tissues become thinner again (as oestrogen decreases).
Virginity is a quality that we all have – it's not a physical thing. It is your choice to share your virginity and experience sexual intimacy with another person – without pressure or impairment (eg, from drugs or alcohol). It can't be 'lost' or 'taken' by someone else. This is really important to understand, because you are in charge of your body and of your sexuality.
You can't tell if someone is a virgin or not based on whether they bleed the first time they have sex. Not all people with vaginas will bleed during their first sexual experience, and that's completely normal. About half will bleed when they first have sex, and half won't bleed.
Bleeding may come from small splits in your hymen or your vagina itself. The bleeding should be lighter than a period and shouldn’t last for more than a couple of days as these tears heal quickly because there is a good blood supply to the vagina.
Some hymens can stretch more than others and will never split or bleed. It is impossible to tell by looking at a hymen whether you've had sexual intercourse or not.
Other factors such as vaginal dryness, not being aroused (turned on), skin conditions (infection or inflammation) and rough sexual contact can also cause bleeding.
There are other causes of bleeding after sex.
- Your hymen doesn't completely cover your vaginal opening – a hole is normal.
- When you have sex, your hymen doesn't 'break or pop' – it stretches, which may cause a small tear.
- You cannot tell by looking at a hymen whether sex has occurred (consensual or non-consensual).
- The size of the opening in your hymen is irrelevant, unless it's so small that it causes pain and stops your menstrual blood coming out through your vagina (then you need to see a healthcare provider).
- Using tampons, bike-riding, doing gymnastics and horse riding are very unlikely to damage your hymen.
- Straddle injuries (falling onto a solid object with your legs open) may cause damage to your hymen and other tissues – see your healthcare provider if this happens.
Virginity, 'first times' and the hymen myth(external link) Just The Facts, NZ
It’s not a cherry and it can’t be popped – exploding the hymen myth(external link) The Spinoff, NZ, 2020
Apps
References
- Congenital anomalies of the female genital tract(external link) O&G Magazine, 2017
- Dietrich JE, Millar DM, Quint EH. Obstructive reproductive tract anomalies(external link) Journal of Pediatric and Adolescent Gynecology 2014;27:396-402.
- Congenital abnormalities of the hymen and vagina(external link) UpToDate, 2024
- Evaluation of sexual abuse in children and adolescents(external link) UpToDate, 2024
- Mishori R, Ferdowsian H, Naimer K, Volpellier M, McHale T. The little tissue that couldn't – dispelling myths about the hymen's role in determining sexual history and assault(external link) Reprod Health 2019;16(1):74.
- Virginity, 'first times' and the hymen myth(external link) Just The Facts, NZ
- Whitley N. The first coital experience of one hundred women(external link) JOGN Nurs. 1978;7(4):41–45.
Mishori R, Ferdowsian H, Naimer K, Volpellier M, McHale T. The little tissue that couldn't – dispelling myths about the hymen's role in determining sexual history and assault(external link) Reprod Health 2019 Jun3;16(1):74.
Diagnosis and management of hymental variants(external link) American College of Obstetricians and Gynaecologists, 2019
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Katie McCullough, Nurse Practitioner, Clinical Lead, STIEF
Last reviewed:





