If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Herd immunity
Key points about herd immunity
- Herd immunity, also known as ‘population immunity’, is when many people in the community are immune to a certain disease.
- This makes it unlikely a disease will spread from person to person.
- Herd immunity is important to protect a community against dangerous and deadly diseases.
- It's reached through vaccination and/or many people catching that particular disease.
Herd immunity, also known as ‘population immunity’, is when a high number of people in the community are immune to a certain infectious disease caused by a bacteria or virus. Being immune to a disease means you can make antibodies which protect you from catching that disease again. Antibodies are proteins that fight off disease.
Herd immunity makes the spread of disease from person to person unlikely. It’s reached through vaccination and/or many people having that particular disease before.
Vaccines train our immune systems to create antibodies. This mimics what happens when we are exposed to the disease itself but, most importantly, vaccines work without making us very unwell. Once you are fully vaccinated, you are far less likely to fall seriously ill with an infection, and less likely to pass the virus to others.
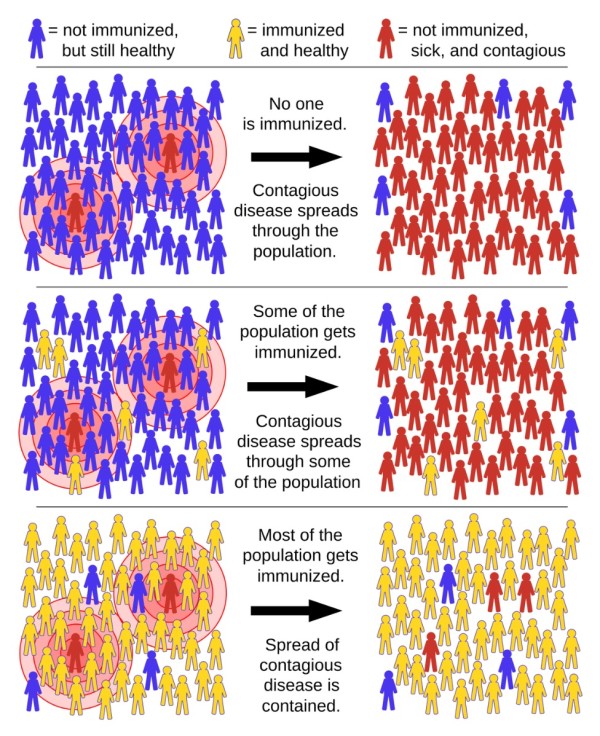
Image credit: Tkarcher via Wikimedia Commons(external link)
Herd immunity threshold
- Herd immunity is especially important to protect a community against dangerous and deadly diseases.
- Usually, a certain percentage of the population must be at risk of getting a disease (not vaccinated and have never had the disease before) for it to spread to others. This is called a ‘threshold proportion’.
- If the number of the population that is immune to the disease (vaccinated or already had the disease) is higher than the threshold proportion then the disease will stop spreading.
- This is known as the ‘herd immunity threshold’.
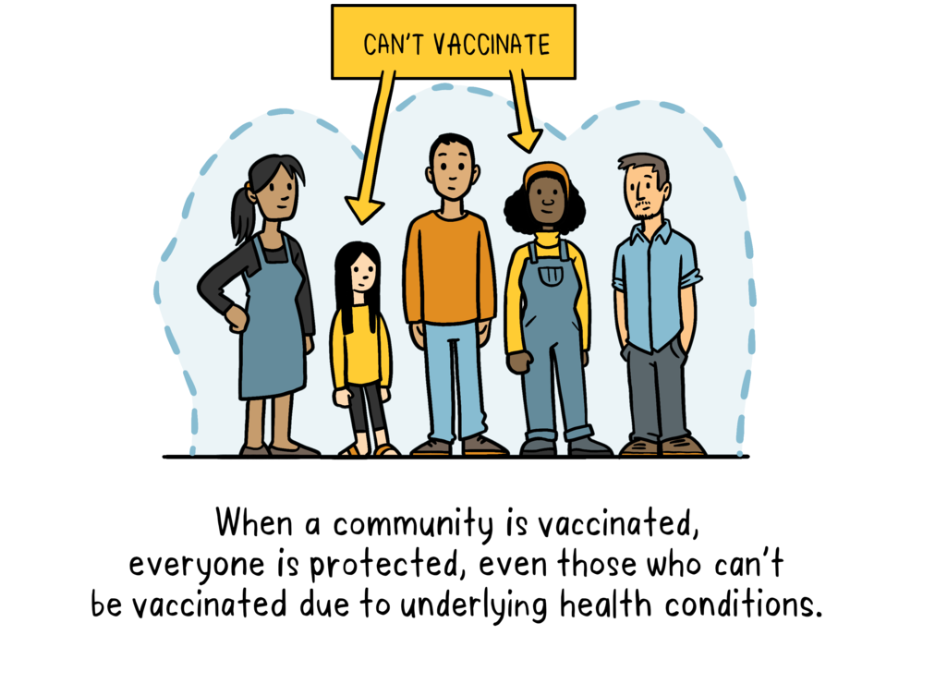
Herd immunity protects the most vulnerable people in our communities. Vulnerable people are those who can't get vaccinated (eg, babies and pregnant women) and people with weakened immune systems, such as those receiving chemotherapy or organ transplants.
When the disease has little opportunity to spread, it's less likely these unvaccinated people will be exposed to it and they can stay safe too.
This is different for each disease. The more contagious a disease is, the greater the number of people need to be vaccinated to stop the spread. For example measles is very contagious and spreads easily. About 95% of a population (95 in 100 people) need to be immune to reach the herd immunity threshold and stop it from spreading. The remaining 5% will then be protected because measles won't spread among people who are immune. For polio the threshold is about 80% (80 in 100 people) because it’s less contagious.
Herd immunity doesn’t work once the percentage of immunised people in a population drops below the herd immunity threshold. An example is if less than 95% of people in the community are immune to the measles. When this happens, a contagious disease can spread very quickly throughout the community.
Humans don’t get strong or long-lasting antibody reactions to some viruses or vaccines. Some viruses change very quickly so that our bodies need to make new antibodies nearly every time we meet them. This means we can catch the disease more than once and the community may not reach a herd immunity threshold. Spread can be slowed down but may not be stopped.
The influenza (flu) virus is like this, which is why a flu vaccine is needed every year. The vaccine works for the person who gets it, but cannot stop yearly flu outbreaks for unvaccinated people in the community.
Protection against COVID-19 should be achieved by vaccination, rather than by exposing people to the virus. This is because the COVID-19 virus can cause serious infection and hospitalisation.
The number of the population that must be vaccinated against COVID-19 to begin herd immunity isn’t known. The COVID-19 virus changes quickly. Humans don’t make a strong or long antibody reaction to the virus or to the vaccines. It’s likely that COVID-19 will need to be controlled with public health measures, such as staying at home when you’re sick, along with booster vaccines and new vaccine development. This is an important area of research.
References
- Coronavirus disease (COVID-19) – herd immunity, lockdowns and COVID-19(external link) WHO
- Herd immunity(external link) Association for Professionals in Infection Control and Epidemiology (APIC), US
- Morens DM, Folkers GK, Fauci AS. The concept of classical herd immunity may not apply to COVID-19(external link) J Infect Dis. 2022 Aug 24;226(2):195–198
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





