Heartburn (Mate taratarawai)
Key points about heartburn
- Heartburn (acid reflux or mate taratarawai) is a burning feeling that happens when acid leaks up from your stomach into your oesophagus (food pipe).
- It's quite common and can be caused or made worse by eating a large meal, being overweight, being pregnant, smoking, some medicines, food and drink.
- Treatment of heartburn includes diet, lifestyle changes and medication.
- Contact your healthcare provider if your symptoms occur frequently or haven’t improved with over-the-counter treatment. Regular heartburn can lead to damage of your oesophagus.

Heartburn is when acid leaks from your stomach into your oesophagus (the tube that carries food from your mouth to your stomach). This can happen when the sphincter (which sits at the junction of your stomach and oesophagus like a valve) doesn't close properly. This could be due to high pressure in your stomach or when your stomach produces too much acid. Most people experience heartburn at some time in their life. The heart is not involved in heartburn.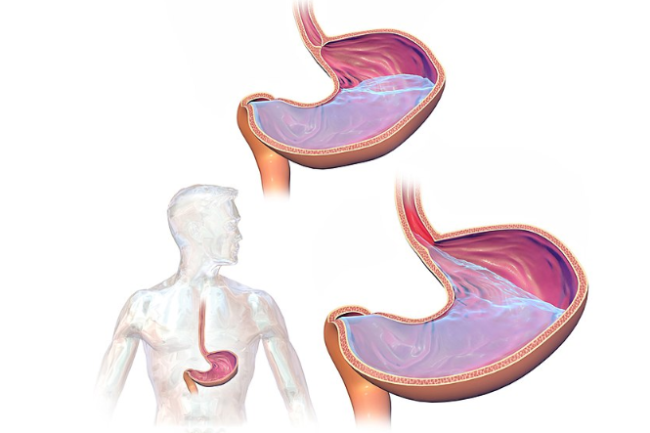
Image credit: commons.wikimedia.org
Indigestion (dyspepsia) is a group of symptoms that describe stomach pain or discomfort experienced after eating. Heartburn is one of these symptoms.
Common signs of heartburn include:
- a burning feeling that rises up from your upper stomach (tummy) or lower chest towards your neck
- acid or undigested food flowing back into your throat or mouth, sometimes causing throat discomfort and bad breath
- upper abdominal (tummy) pain or discomfort
- cough or hiccups that keep coming back
- bloating or nausea (feeling sick).
Occasional heartburn is usually nothing to worry about but if heartburn is severe or not treated it can lead to the following conditions:
- Gastro-oesophageal disease (GORD): This is an inflammation of the lining of your oesophagus.
- Reflux oesophagitis: Frequent or an extended period of heartburn can inflame your oesophagus because it gets 'burnt' by the acid leaking up (refluxing) from your stomach.
- Respiratory problems: People with heartburn occasionally develop respiratory problems (eg, asthma, chronic cough, pneumonia) or experience choking at night or a sore throat in the morning.
Click the image below to visit the website, scroll down to see the video on acid reflux or GERD, then click play.
(Cleveland Clinic, NZ, 2019)
There are a number of lifestyle changes you can make to reduce symptoms of heartburn and reduce the need for medicines.
- Eat small amounts of foods often rather than larger meals 3 times a day. Don’t overeat, and chew well.
- Avoid foods that trigger symptoms. These include common foods and drinks such as fatty foods, spicy foods, chocolate, coffee, cola drinks, orange juice or alcohol.
- Quit smoking. Smoking causes acid reflux. Read more about quitting smoking.
- Stay upright after a meal. Wait at least 3 hours after eating before lying down or going to bed.
- Lose weight if you are overweight. Excess weight puts pressure on your stomach, causing acid to go back up your oesophagus.
- Raise the head of your bed by 10–20 cm so your head is higher than your stomach. Avoid sleeping on your right side.
- Avoid or reduce the use of non-steroidal anti-inflammatories (NSAIDs). Talk to your pharmacist or family doctor for advice on pain relief.
- Avoid tight clothing around your waist.
- Manage stress.
Call 111 for emergency help if you experience the following:
- difficulty swallowing
- vomit containing fresh blood or dark granules
- ongoing vomiting
- pain on swallowing
- chest pain or tightness
- unexplained weight loss
- black poos
These may be warning signs for more serious conditions such as gastric (stomach) ulcers or, very rarely, stomach or oesophageal cancer. Your doctor will also check that your symptoms are not caused by a problem with your heart.
Contact your healthcare provider if you have any of the following:
- heartburn on most days for 3 weeks or more
- your symptoms have not improved after 4 weeks of treatment with medicine
- your symptoms get more frequent or severe
- you develop regular heartburn for the first time and you are aged over 50 years (over 45 years if you are Māori, Pacific Peoples or Asian).
Apps reviewed by Healthify
You may find it useful to look at some Nutrition, exercise and weight management apps and Quit smoking apps.
- being overweight
- eating large meals and overeating
- smoking
- certain food and drinks such as fatty foods, spicy foods, chocolate, coffee, cola drinks, orange juice or alcohol
- stress.
Medicines
The most common type of medicine that causes heartburn are non-steroidal anti-inflammatory (NSAID) medicines (eg, aspirin, ibuprofen, diclofenac and naproxen). They can cause heartburn and indigestion (dyspepsia).
Pregnancy
Heartburn during pregnancy is common from 27 weeks onwards when your womb (uterus) pushes up against your stomach putting pressure on it. Read more about pregnancy.
Hiatus hernia
This is a condition where one of the organs in your abdomen (tummy) pushes up into your chest area through an opening in your diaphragm. Read more about hiatus hernia.
To make a diagnosis of heartburn, your healthcare provider will talk to you about your symptoms.
Mild and occasional heartburn
Usually no test is needed. Lifestyle changes and pharmacy medicines can be used as treatment.
Frequent or regular heartburn
Your doctor may do further tests to find out how severe your heartburn is or if there is any damage to your oesophagus.
Tests may include:
- Blood tests – complete blood count (CBC), ferritin and C-reactive protein (CRP)
- H. Pylori – faecal test
- pH monitoring – this test involves using an acid monitor (a thin tube with a sensor at one end) to measure acidity levels in your oesophagus.
- Other tests – an endoscopy, chest x-ray or ECG may be done to rule out other conditions with similar symptoms.
As well as using self-care methods, there are 2 main types of medicines for treating heartburn:
- Antacids – provide fast relief by lowering the level of acid in your stomach. However, they don’t heal oesophageal damage or prevent heartburn from happening again. Antacids can be bought from a pharmacy. Read more about antacids.
- Proton pump inhibitors – block the stomach making acid which helps to heal any damage in your oesophagus. Examples include omeprazole and lansoprazole. You can buy omeprazole from your pharmacy. Proton pump inhibitors should not be taken for more than 4 to 8 weeks. Read more about proton pump inhibitors.
- Histamine blockers – which reduce the production of stomach acid and help to heal stomach ulcers, eg, famotidine and cimetidine)
If you're pregnant, ask your doctor, nurse or pharmacist to find out whether these medicines are safe for you to take.
Surgery
Surgery is an option for a few people with persistent and severe symptoms if lifestyle changes and various medicines haven't helped. Surgery aims to provide a cure by tightening the oesophageal sphincter at the top of your stomach. But, as with all surgery, there are associated risks. Talk to your healthcare provider to find out the best treatment options for you.
Heartburn and reflux(external link) Choosing Wisely, NZ
Heartburn(external link) Health Direct, Australia
Heartburn and acid reflux(external link) NHS, UK
Indigestion and heartburn in pregnancy(external link) NHS, UK
Acid reflux and oesophagitis(external link) Patient Info, UK
Apps
Nutrition, exercise and weight management apps
Quit smoking apps
References
- Heartburn and reflux(external link) Choosing Wisely, NZ, 2016
- Acid reflux and oesophagitis(external link) Patient Info, UK 2020
- Managing dyspepsia and heartburn in general practice – an update(external link) BPAC, NZ, 2011
Clinical pathways and guidelines
Managing dyspepsia and heartburn in general practice - an update(external link) BPAC, NZ, 2011
Managing heartburn undifferentiated dyspepsia and functional dyspepsia in general practice(external link) BPAC, NZ, 2007
Management of dyspepsia and heartburn(external link) NZ Guidelines Group, Ministry of Health, 2004
Increasing primary antibiotic resistance and ethnic difference in eradication rate of helicobacter-pylori infection in NZ – a new look at an old enemy(external link) NZ Medical Journal, 2013
Gastro-oesophageal reflux disease and dyspepsia in adults – investigation and management(external link). NICE, UK, 2014
Continuing professional development
eLearning
Gastro-oesophageal reflux disease – diagnosis and treatment(external link) The Royal New Zealand College of General Practitioners modules, BMJ Learning
Podcast
Dyspepsia and heartburn – Dr. Paul Frankish(external link)
Dr Paul Frankish talks about dyspepsia and heartburn. Paul is a Consultant Gastroenterologist and is Endoscopy Lead for the Waitemata bowel screening pilot. His special interests are in bowel screening, advanced endoscopy and also in training. Paul is an honorary senior lecturer in Gastroenterology at the University of Auckland.
Apps
Nutrition, exercise and weight management apps
Quit smoking apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Tracey Xu, RN, PGHealSc, Mauri Ora Student Health and Counselling, Victoria University of Wellington
Last reviewed:
Page last updated: