If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Ulcerative colitis | Mate kōpiro nui
Key points about ulcerative colitis
- Ulcerative colitis is an inflammatory bowel disease that causes swelling and ulcers in the lining of the large intestine (colon).
- It's a long-term condition that can have a significant impact on everyday life.
- Common symptoms include bloody diarrhoea (runny poo), and frequent or urgent poo.
- Ulcerative colitis may occur at any age, but most commonly occurs for people at 18–35 years.
- Treatment involves medicines but surgery may be needed if it's severe.

Video: Mayo Clinic Explains Ulcerative Colitis
The large intestine, or colon, is the final part of your digestive system (see the image below). By the time food has passed through the 6.5 metres of your small intestine and reaches your colon, most of it has been absorbed and only waste products are left. It is the job of your colon to absorb the excess water, as well as some fibre and potassium, from the waste and move the waste to the rectum. This becomes your stools (poos).
Inflammatory bowel disease (IBD) is a medical term used to describe a group of conditions in which the intestine becomes inflamed (red and swollen). There are two major types of IBD and they require different treatments.
- Crohn's disease can occur in any part of your intestine.
- Ulcerative colitis only affects your large intestine (colon). Small ulcers can develop on the colon's lining, and can bleed, produce pus and become inflamed.
Note that IBD should not be confused with irritable bowel syndrome (IBS), which is a different condition requiring different treatment.
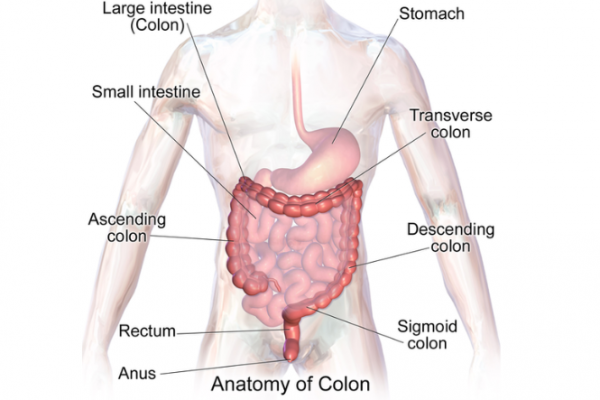
Image credit: Blausen Medical Gallery via Wikimedia Commons
The exact cause of ulcerative colitis is unknown. The following possible causes have been suggested:
- Immune system
- Ulcerative colitis is thought to be a type of autoimmune disease, in which the body's immune system (infection fighting system) malfunctions and attacks the tissues of the bowel. This results in swelling and redness (inflammation) of body tissue in the infected area. It’s also been suggested that no infection is involved and the immune system may just malfunction by itself, or that there’s an imbalance of bacteria within the bowel.
- Genes
- It also seems inherited genes are a factor in the development of ulcerative colitis. If your first degree relative (parent, brother, sister, child) has colitis, this can double your lifetime risk. Levels of ulcerative colitis are also a lot higher in people of European or African descent, which also suggests that genetics are a factor.
The most common symptoms are bloody diarrhoea (blood on runny poo), frequent passing of stools and/or an urgent need to pass stools (poos). Occasionally some people may have pain in the lower abdomen (tummy/puku area).
More severe symptoms include weight loss, anaemia, loss of appetite, tiredness, feeling low in mood and slower than usual growth (which is more noticeable in younger people).
The severity of symptoms varies between people and depends on how much of the rectum and colon is inflamed and how bad the inflammation is. Some people experience their first ulcerative colitis-like symptoms when they are attempting to stop smoking but this goes away with time.
If you have any symptoms of ulcerative colitis and are not diagnosed or your medication is not working well for you, see your GP.
Flare-up
Some people may go for weeks or months with very mild symptoms, or none at all (remission), followed by periods where the symptoms are particularly troublesome (flare-ups or relapses). In some cases, a flare-up can be linked to specific cause such as a change of medication or a certain food, however in many cases a specific cause is not found.
During a flare-up, some people with ulcerative colitis also experience symptoms elsewhere in their body. For example, some people develop:
- painful and swollen joints (arthritis)
- mouth ulcers
- areas of painful, red and swollen skin
- irritated and red eyes.
Ulcerative colitis can occur at any age, but it is often diagnosed in people aged 18 to 35 years old. Men and women seem to be equally affected.
If you have ulcerative colitis you may also have another immune condition such as asthma, psoriasis or type 1 diabetes. So if you have an immune condition and symptoms of ulcerative colitis, see your GP.
Ulcerative colitis is often diagnosed using a mixture of methods. It is best to talk to your doctor so they can check if your symptoms are caused by another condition instead. Your doctor will ask you about your symptoms and medical history. They may also want to:
- Take a blood sample to check for anaemia and check the levels of your infection fighting (immune) cells. The test may also include checking for test C-reactive proteins (CRP) to check for the presence of inflammation or infection in your body.
- Get a stool (poo) sample from you to check for inflammation and signs of an infection, eg, gastroenteritis.
- Arrange a test on your lower bowel called a sigmoidoscopy. A narrow tube containing a camera and a light is passed through your anus into the lower bowel. This allows a specialist to look at the lining of your colon. Sometimes a small piece of tissue is removed (biopsy) so it can be examined more closely in a laboratory.
- Arrange a colonoscopy. This allows a greater length of your colon to be examined to rule out Crohn’s disease (which has similar symptoms to ulcerative colitis).
If you have been diagnosed with ulcerative colitis, your doctor will often want to continue many of the tests above so they can monitor your condition over time. As people with ulcerative colitis have a higher chance of getting cancer of the colon, especially if the disease begins before the age of 15 or continues for longer than 10 years, regular colonoscopies can help detect this cancer.
The main aim of treatment for ulcerative colitis is to stop inflammation in the colon, to prevent flare-ups and to keep you in remission (without symptoms). The kind of treatment depends on the type of symptoms and how bad they are.
Medication
Medicines are used to control the inflammation in your colon and to reduce your body’s immune response. Often medicines are prescribed in a ‘stepped’ approach, depending on your response and symptoms. Read more about the medications used for ulcerative colitis.
Nutrition and diet
Although diet does not cause ulcerative colitis, there may be times when changes in your eating habits can help control your symptoms and prevent flare-ups. Many people with ulcerative colitis find it helpful to keep a diary of daily food and drink intake to see which drinks or foods may be linked to worsening symptoms. Each person with ulcerative colitis is different, so try to find out what works for you.
Other useful tips are:
- Try to maintain a healthy varied overall diet.
- Increase your intake of natural sources of omega-3 fatty acids, eg, salmon or flax/chia seeds.
- Reduce your consumption of red and processed meat. Remember to supplement your diet with iron or protein rich foods so you don’t develop anaemia.
- Speak to a dietitian for advice if you are struggling to maintain a well-balanced diet or if you have a lot of inflammation that means you are not absorbing as many nutrients.
- Try a gluten free diet for a while.
- Drink plenty of water – especially when you have flare-ups. The water you lose through diarrhoea can make you dehydrated. Try to avoid caffeine and alcohol, as these will make your diarrhoea worse, and fizzy drinks, which can cause flatulence (gas).
- Take food supplements – ask your doctor if you need food supplements, as you might not be getting enough vitamins and minerals in your diet.
Surgery
If you have severe ulcerative colitis that does not respond to drug treatment or affects your quality of life, having surgery to remove your colon or part of your bowel is an option.
Other treatments
- Stopping smoking: All people with ulcerative colitis are recommended to stop smoking. People who smoke are more likely to need surgery than non-smokers.
- Keep up to date with vaccinations: People with ulcerative colitis are often immunocompromised or are taking immune suppressing medicines.
- Exercise: Weight bearing exercise can help reduce tiredness and helps improve your bone health especially if you are taking steroids such as prednisone.
- Herbal supplements:
- Turmeric: Some people find that the anti-inflammatory properties of turmeric can help. However, as with all herbal products, check with your pharmacist to see if it interacts with any medicines you are taking and what dose to take.
- Cannabis based products: There is insufficient evidence to support the use of cannabis based products in ulcerative colitis.
- Helminth therapy: There are several studies which have looked into the use of helminth therapy for achieving remission in ulcerative colitis. There are no firm conclusions on this therapy and the therapy is not approved in Aotearoa New Zealand.
- Probiotics: There is some evidence that taking probiotics (live bacteria and yeast that are good for your gut) as well as medicines may be useful. It has not been proved.
Living with a condition like ulcerative colitis, especially if your symptoms are severe and unpredictable, can be a frustrating and isolating experience. Remember that ulcerative colitis does not have to dominate your life.
- Talking to others with the condition can provide support and comfort. Crohn's and Colitis NZ(external link) provides information on where you can find help and support.
- Remember to take a sick day when you need to.
- If you have unpredictable bowel movements in the morning and worry about getting to work on time, speak to your employer to see if you can change your working hours or work from home.
- Plan your trip so you know where the nearest bathroom is.
- This "I Can't Wait!" toilet card(external link) from Crohn's and Colitis NZ may help you gain access to a toilet quickly.
- Connect with others who have ulcerative colitis. Even though everyone's experience will be different, it may help to share ideas.
The support of friends and whānau can make a huge difference in helping someone with ulcerative colitis live well with their condition.
Image credit: Pixabay
Here are some tips:
- Ulcerative colitis is fluctuating and unpredictable: You may be confused when you see your friend or relative out and about when just last night they cancelled plans with you, but symptoms can change significantly from one moment to the next. Be understanding when they can't make it to an event. It’s also possible that their ulcerative colitis has caused a strain on their finances – they may not be able to work full-time or in stressful roles while they’re unwell, or they may struggle with prescription costs and transport to hospital.
- Avoid blaming stress: Although stress could be a contributing factor, it does not help to say ‘try being less stressed’.
- Be there to listen if they want to talk: Sometimes they would prefer to just carry on as normal and not talk about their illness, but other times they may appreciate someone to open up to.
- Help boost their confidence if they start to look different: Surgery scars or fluctuating weight can have a negative effect on body image, so they may appreciate reassurance that you don’t see them differently.
- Don't judge their food choices: It’s understandable to think that gut issues may have been caused by poor diet. However, there’s no conclusive evidence that any particular food or additive can cause or cure ulcerative colitis.
- Keep them in the loop when they’ve missed something: If they’re regularly missing out on work, school or social events because of ill health, they can feel isolated, which can have a negative effect on their mental health.
Apps reviewed by Healthify
You may find it useful to look at some Long-term condition apps, Digestive health apps, and Mental health and wellbeing apps.
Crohn's and Colitis NZ (external link)(external link)
Freephone 0800 ASK IBD. Support, advice and information to interested individuals and people who have Crohn's disease or ulcerative colitis and their families or caregivers. Crohn's and Colitis NZ also provides educational material to medical professionals and organisations within New Zealand.
Video: Living with ulcerative colitis – Louise Thompson
This video may take a few moments to load.
(Crohn's & Colitis UK, 2019)
Video: MY LIFE WITH UC - What Is Ulcerative Colitis?
This video may take a few moments to load.
(Canadian Digestive Health Foundation, Canada, 2016)
Video: Leaving Home - University with Crohn's and Colitis
This video may take a few moments to load.
(Crohn's & Colitis UK, 2017)
Video: Schooling with Crohn's and Colitis
This video may take a few moments to load.
(Crohn's & Colitis UK, 2017)
Crohn's & Colitis NZ(external link) (includes real stories and groups to connect with others)
Crohn's & Colitis UK(external link)
Living with inflammatory bowel disease – handbook(external link) Crohn's & Colitis NZ
Apps
Long-term condition apps
Digestive health apps
Mental health and wellbeing apps
Resource
Living with inflammatory bowel disease – handbook(external link) Crohn's & Colitis NZ
References
- Ulcerative colitis(external link) Patient Info UK, 2020
- Inflammatory bowel disease – a focus on Crohn's disease and ulcerative colitis(external link) BPAC, NZ, 2021
- Ulcerative colitis clinical pathway(external link) National Institute of Clinical Excellence (NICE), UK
- Ulcerative colitis(external link) Mayo Clinic, US, 2021
- Inflammatory bowel disease – a focus on Crohn's disease and ulcerative colitis BPAC, NZ, 2021
- Ulcerative colitis clinical pathway(external link) National Institute of Clinical Excellence (NICE), UK
- Sexual and reproductive health for individuals with inflammatory bowel disease(external link) Faculty of Sexual and Reproductive Healthcare of the Royal College of Obstetricians and Gynaecologists (FSRH)
- BMJ Learning – The Royal New Zealand College of General Practitioners Modules(external link) [free for RNZCGP members, requires registration]
- BSG consensus guidelines on the management of Inflammatory Bowel Disease in adults(external link) British Society of Gastroenterology , UK
- Webinar – inflammatory bowel disease(external link) February 2018, Dr Alasdair Patrick
- Sinopoulou V, Gordon M, Dovey TM, et al. Interventions for the management of abdominal pain in ulcerative colitis(external link) Cochrane Database Syst Rev. 2021;7(7):CD013589
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Derek JY Luo, MBChB (Otago) FRACP, consultant gastroenterologist
Last reviewed:
Page last updated:





