You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Post-exposure prophylaxis (PEP)
Also called emergency HIV prevention
Key points about post-exposure prophylaxis (PEP)
- Post-exposure prophylaxis is emergency HIV prevention.
- It refers to medicines that can prevent HIV after a possible exposure.
- PEP must be started within the 72 hours (3 days) after a possible exposure to HIV. Ideally, PEP is started within 24 hours of exposure.
- You can get PEP from medical centres, urgent care/after hours services and hospital emergency departments.

PEP stands for post-exposure prophylaxis, and is also called emergency HIV prevention. It refers to medicines that prevent HIV after a possible exposure. If you're HIV negative and think you may have been exposed to HIV (during sex, or by sharing injection equipment) you should go to your local after-hours clinic, or to the emergency department of your nearest hospital or contact your GP, and ask for PEP (see who would benefit from taking PEP below).
The sooner you start PEP, the better
- PEP is most effective when started within 24 hours, but it must be started within 72 hours of exposure.
- The longer you wait, the greater the chance that PEP won’t work.
- PEP usually isn’t given more than 72 hours (3 days) after exposure as studies show it's unlikely to be effective.
- Many pharmacies have stock or can usually order it in for you within 24 hours. See Healthpoint(external link) for pharmacies that keep PEP. Other providers (eg, emergency departments) may offer access to PEP.
Asking for PEP
When going to ask for PEP, it could be a good idea to take a friend or loved one with you for support.
When you ask for PEP the doctor or nurse will need to ask you detailed questions about what happened where you may have been exposed to HIV, eg, sex without a condom or sharing injecting equipment. Be clear and honest when talking to them about what has happened and why you feel you're at risk of HIV infection. This information will help them assess whether PEP is suitable for you and whether you need a 2-medicine or 3-medicine regimen.
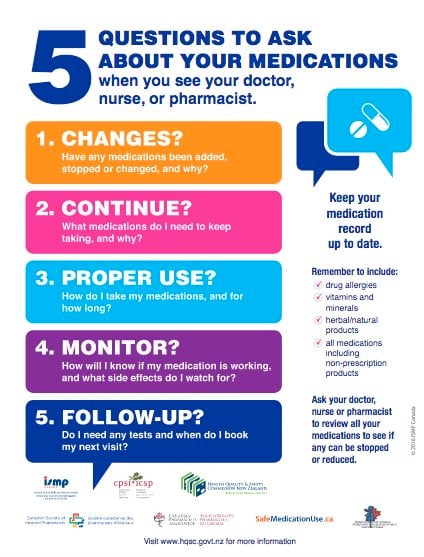
Let them know about any other medicines you are taking or any medical conditions you have. Also let them know if you're pregnant or breastfeeding or think you might be pregnant.
There are 2 options for PEP
- 2-medicine regimen: This involves taking ONE tablet, once daily, for 28 days. Each tablet is made up of the antivirals tenofovir disoproxil and emtricitabine.
- 3-medicine regimen: This involves taking TWO tablets, once daily, for 28 days. One of the tablets is made up of the antivirals tenofovir disoproxil and emtricitabine and the other tablet is dolutegravir.
The choice will depend on the risk of transmission.
Note: You must take all of your prescribed doses to make sure the medicine is as effective as it can be.
PEP is free for those eligible for publicly funded healthcare in Aotearoa New Zealand who meet one or more of the following PHARMAC criteria:
- You have had anal intercourse or receptive vaginal sex with someone living with HIV with an unknown or detectable viral load.
- You have had anal intercourse with someone from a high HIV prevalence country or high HIV risk group with an unknown HIV status.
- You have shared intravenous injecting equipment with someone living with HIV.
- You have had non-consensual intercourse and your doctor thinks PEP would be suitable.
If taken within 72 hours after possible exposure, PEP is effective in preventing HIV. But to be safe, you should take other actions to protect your partners while you are taking PEP. This includes always using condoms with sexual partners and not sharing needles, syringes, or other equipment to inject drugs.
To find out if PEP is right for you, talk to your healthcare provider. You can also find out more about PEP on the Burnett Foundation Aotearoa(external link) website.
Note: If you don't meet the criteria for funded PEP, ask your healthcare provider about self-funding. If it's a suitable option, they can still write a prescription and you can pay for your own PEP pills at the pharmacy. Prices may differ slightly between pharmacies.
Interactions with other medicines
PEP can interact with some medicines, herbal supplements and rongoā Māori, This includes anti-inflammatories that you can buy at your supermarket or pharmacy. Anti-inflammatories include ibuprofen (Nurofen) or diclofenac (Voltaren). Always check with your doctor or pharmacist before starting PEP and before starting any new products.
Side effects of PEP
Like all medicines, PEP can cause side effects, although not everyone gets them. Often side effects improve as your body gets used to the new medicine. Common side effects are generally mild and can include:
- nausea (feeling sick)
- vomiting (being sick)
- tummy pain
- flatulence (gas and wind)
- diarrhoea (runny poo)
- headache.
Blood tests
Once you have started PEP, you will need to book follow-up HIV tests to see whether PEP has been successful. Your doctor will advise you on when it's best to do this.
Both PEP and PrEP are HIV prevention antiviral medicines taken by people who don't have HIV.
- PEP is post-exposure prophylaxis, and is an emergency HIV prevention if you've been exposed to HIV. The most common reasons for needing PEP are:
- sex without a condom with a person who has, or might have, HIV
- a condom breaking or slipping off during sex
- sharing needles or syringes with a person who has, or might have, HIV.
- PrEP stands for pre-exposure prophylaxis and is used to prevent HIV before exposure. If you find that you've had to start PEP, then you may want to consider using PrEP in future. Your doctor can start you on PrEP after your course of PEP. Learn more about PrEP.
PEP(external link) Burnett Foundation Aotearoa, NZ
HIV Basics(external link) PEP Body Positive New Zealand
References
- PrEP and PEP guidelines for Aotearoa New Zealand(external link) NZSHS and Burnett Foundation Aotearoa, NZ, 2023
Workforce development(external link) Burnett Foundation Aotearoa has online modules and resources for clinicians
PrEP and PEP guidelines for Aotearoa New Zealand(external link) NZSHS and Burnett Foundation Aotearoa, 2024
Prescribing HIV post-exposure prohylaxis (PEP) in Aotearoa New Zealand(external link) NZSHS and Burnett Foundation, 2023
B-QuiCK – HIV post-exposure prophylaxis (PEP)(external link) BPAC, NZ, 2024
HIV pre- and post-exposure prophylaxis – (external link)a guide for primary care(external link) BPAC, NZ, 2024
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland; Cameron Leakey, Research Officer, Burnett Foundation Aotearoa
Last reviewed:
Page last updated:





