Wishing everyone happy holidays and a joyful New Year from the Healthify team. Don't forget to Slip, Slop, Slap and Wrap!
Myelodysplastic neoplasms
Also known as MDS or myelodysplasia
Key points about myelodysplastic neoplasms
- Myelodysplastic neoplasms (MDS) are a group of rare, but potentially serious, neoplastic or “cancerous” blood disorders.
- MDS is a group of blood disorders where blood cells aren't made properly. MDS is characterised by low blood cell counts and/or blood cells that don't look normal.
- MDS is most common in people over 70 years of age, but can occur at any age.
- Symptoms generally occur as a result of low blood cell counts and include fatigue and low energy levels, repeated infections, and bruising or bleeding more often than usual.
- MDS can’t usually be cured. Treatment aims to slow the progression of MDS, relieve symptoms and manage associated conditions such infection and blood loss.

Myelodysplastic neoplasms (MDS) is a term encompassing a group of malignant or cancerous blood conditions in which your blood cells don’t form or work properly. MDS develops because there’s something wrong with your bone marrow (the part of your bones where blood cells are made) resulting in reduced or abnormal blood cell production. This in turn leads to low numbers or “abnormal looking” blood cells in your blood.
MDS is a rare, but potentially serious condition. It’s most common in people over 70 years of age, but can occur at any age. MDS is classified as low risk or high risk based on blood and bone marrow results and may progress quickly or slowly over time. MDS, in particular “high risk MDS” may develop into acute leukaemia.
The bone marrow is your body’s factory for the cells in your blood. Healthy bone marrow makes new immature blood cells that mature into red blood cells, white blood cells and platelets over time.
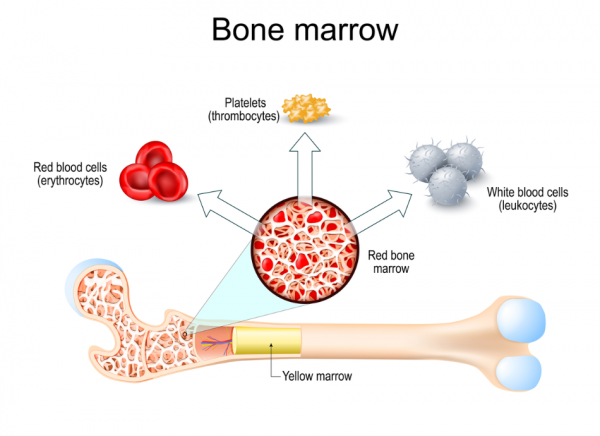
Image credit: Depositphotos
In people with healthy blood:
- the red blood cells carry oxygen around your body
- the white blood cells help fight infection
- the platelets help your blood to clot and prevent bleeding.
If you have (MDS), something has gone wrong in your bone marrow, and blood cells don't develop and mature properly. This leads to low blood counts and/or the presence of dysplastic or “abnormal looking” blood cells.
In most cases, the cause of MDS isn’t known. However, you may be at increased risk of MDS if:
- you’re over 60 years of age
- you’ve had chemotherapy or radiotherapy treatment in the past, eg, to treat cancer
- you’ve been exposed to certain chemicals, eg, benzene, or heavy metals such as mercury or lead
- you’re a cigarette smoker.
Some people have a genetic condition that increases their risk of developing MDS.
Some people may not have any signs or symptoms of MDS at all, but you may find out you have MDS after a blood test you had for a different reason.
However, over time you may notice:
- fatigue (exhaustion or lack of energy)
- shortness of breath
- paleness of your skin (you can become anaemic if your red blood cells are affected)
- that you bruise or bleed easily/more often than usual, eg, nosebleeds or bleeding gums
- red pinpoint-sized spots just under your skin (caused by bleeding)
- that you're more prone to infections (if your white blood cells are affected).
You should seek medical advice if you:
- have a fever (a temperature of 38°C or above)
- have symptoms of infection such as shivering, coughing up yellow or green phlegm, fatigue or extreme tiredness
- have bleeding that won't stop (if your platelets are affected).
Your doctor will talk to you about your symptoms, examine you and arrange tests to confirm whether you have a myelodysplastic neoplasm (MDS). You may be referred to a haematologist – a doctor who specialises in blood disorders.
Possible tests include:
- Full blood count: This is done to count the different blood cells (red cells, white cells, and platelets) in your blood and to assess whether any are unusually sized or shaped. In MDS, the number of the various blood cells may be reduced, the blood cells may looks abnormal or there may be a combination of both.
- Bone marrow biopsy: This is a test in which bone marrow (the liquid portion inside the bone) and a small core of the bone is removed using a thin needle, and examined under a microscope. It’s usually taken from the back of your hip bone.
There are different types of myelodysplastic neoplasms (MDS) depending on the type of blood cell(s) involved and whether any genetic changes have occurred. One, or more than one, type of blood cell may be affected, and some people may have a mutation (change) in their DNA causing changes in their blood cell chromosomes.
Once a diagnosis of MDS is confirmed from a bone marrow biopsy, it's sub-classified into 1 of several disease groups based on:
- the number of cell types that are affected
- genetic or chromosome changes, and
- the presence of absence of various mutations.
Based on these results, the condition is also categorised as low or high-risk disease.
Testing of your blood and bone marrow can help predict the likely course of your MDS. Some types of MDS stay mild (or indolent) for years, but others are more serious.
The main focus of treatment is to:
- relieve your symptoms
- slow the progression of the disease and prevent any complications
- help you live as normal a life as possible.
Your treatment plan may include 1 or more of the following.
- Active monitoring: This is sometimes called ‘watch and wait’. If you don’t have any symptoms and your blood counts are stable, you may not need treatment right away. Your healthcare provider will recommend that you have regular blood tests so they can monitor the progress of your MDS.
- Chemotherapy and other targeted drug therapy: This is used to kill the abnormal or cancerous blood cells and allow normal cells to be made
- Bone marrow transplant: This is also called stem cell transplant. This is when your bone marrow is replaced with bone marrow from a healthy donor. This may cure MDS, but not everyone is suitable for bone marrow transplantation. Read more about bone marrow transplantation.
- Supportive care: This may include treatments such as:
- blood transfusions to increase levels of healthy red blood cells in your blood
- growth factors to help your bone marrow make more blood cells
- medicines such as antibiotics to treat infections.
The type of treatment you receive will depend on:
- the type of MDS you have
- whether you have anaemia, bleeding or infections
- whether you’ve had previous chemotherapy or radiotherapy
- your age and general health
- your prognosis (the likely progression of your disease, eg, your risk of developing acute myeloid leukaemia).
MDS is a chronic (long-term) condition, which can be life-altering, and your healthcare team may also talk to you about palliative care(external link). The palliative care team can help with managing your symptoms and any side effects you have from the treatment you’re receiving. They can also provide you and your whānau with ongoing help to support your overall health and wellbeing.
If you have myelodysplastic neoplasm (MDS) with a low number of white blood cells, you’re at increased risk of infection, which may be serious.
Do the following to reduce your risk of infections.
- Wash your hands often and thoroughly with warm soapy water especially before eating or preparing food.
- Take care with food – thoroughly cook meat and fish, wash and peel fruit and veges, avoid fruit and veges that you can’t peel, avoid raw foods.
- Stay away from people who are sick, including family members and co-workers.
- Vaccines can prevent infections so talk to your healthcare provider about getting vaccinated against diseases such as influenza, COVID-19 and shingles.
If you have MDS with a low number of platelets, things you can to reduce bruising and bleeding include:
- use a soft toothbrush
- don’t floss your teeth
- use an electric razor rather than a razor blade
- avoid contact sports
- move carefully so you don’t bump into things
- wear protective gloves when working round the house or garden.
If you’re being actively monitored (‘watch and wait’), get your regular blood tests and do your best to keep active and maintain healthy lifestyle habits including:
- regular exercise
- healthy eating
- maintaining a healthy weight
- doing things to reduce your stress levels
- stopping smoking
- stopping or reducing your alcohol intake
- using a high-factor sunscreen and wearing a hat outdoors to protect against skin cancer.
Having a blood cancer such as MDS can be physically and emotionally stressful.
Leukaemia and Blood Cancer New Zealand(external link) is an organisation that’s committed to improving the quality of life for patients and their families/whānau living with blood cancers. They have dedicated Support Services Coordinators who are available to provide support and information to patients and their families/whānau.
Myelodysplastic neoplasm (MDS) is a potentially serious condition that can be life-threatening.
Complications of MDS include:
- anaemia due to low numbers of red blood cells
- recurrent infections due to low numbers of white blood cells
- bleeding that’s hard to stop due to low numbers of blood-clotting platelets
- increased risk of cancer such as acute myeloid leukaemia.
MDS affects people in different ways. Talk to your healthcare provider about your individual management and outlook.
What is MDS?(external link) MDS UK Patient Support Group, UK
Brochures
Myelodysplastic syndromes (MDS) – a guide for patients, families and whānau(external link) Leukaemia and Blood Cancer New Zealand
Blood cancers and conditions – Māori(external link) Leukaemia and Blood Cancer New Zealand. Also available in Samoan, Tongan, Korean, Hindi, Chinese (simplified), Chinese (traditional)
Myelodysplastic syndromes (MDS) – a guide for people affected by myelodysplastic syndromes(external link) MDS UK Patient Support Group and Leukaemia Care, UK
References
- Myelodysplastic syndrome (myelodysplasia)(external link) NHS, UK, 2021
- Myelodysplastic syndromes(external link) Mayo Clinic, US, 2022
- Myelodysplastic syndrome (myelodysplasia)(external link) Cleveland Clinic, 2023
- Myelodysplastic syndromes (MDS) – a guide for patients, families and whānau(external link) Leukaemia and Blood Cancer New Zealand
Myelodysplastic syndromes(external link) Patient, UK, 2022
Brochures
Myelodysplastic syndromes (MDS) – a guide for patients, families and whānau
Leukaemia and Blood Cancer New Zealand
Blood cancers and conditions – Māori
Leukaemia and Blood Cancer New Zealand
Also available in Samoan, Tongan, Korean, Hindi, Chinese (simplified), Chinese (traditional)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Peter Ou, GP, FRNZCGP, Auckland; Dr Anna Elinder Camburn, Consultant Haematologist, Auckland
Last reviewed: