Wishing everyone a safe and happy Christmas and New Year – Meri Kirihimete from the Healthify team.
Meningococcal disease
Can cause meningitis and sepsis
Key points about meningococcal disease
- Meningococcal disease is a bacterial infection that can lead to serious illnesses including meningitis and sepsis which can be deadly.
- Early symptoms can be similar to influenza (the flu) but quickly get much worse.
- Meningococcal disease can be treated with antibiotics.
- Early treatment is very important. Don't wait – take action!

If you or someone in your household is sick with one or more of the symptoms below, don't wait, act immediately. Ring a doctor, medical or after-hours centre or the free Healthline number (0800 611 116) right away, day or night. If it's an emergency, call 111. |
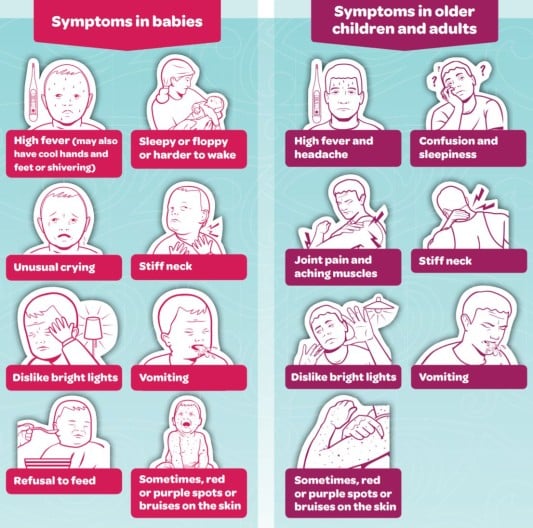
Image credit: Health Promotion Agency, NZ
What is meningococcal disease?
Meninogococcal disease is caused by meningococcal bacteria. There are several different types of meningococcal bacteria including A, B, C, Y and W. Most cases are caused by the B type. W type is the second most common and was the cause of the outbreak in Northland 2018/2019.
Usually, the bacteria sit harmlessly in the back of healthy people’s noses and throats and are not passed on to others. The illness happens when these bacteria enter the bloodstream to cause septicaemia (infection in your blood, also known as bacteraemia) or meningitis (inflammation of the membrane covering your brain). Sometimes severe infection can also occur in your joints, throat, lungs or intestines.
Video: Meningococcal disease
Watch this video by clicking on the image. (external link) (Immunisation Advisory Centre, NZ, 2017)
(external link) (Immunisation Advisory Centre, NZ, 2017)
Meningococcal disease can look like influenza (the flu) in its early stages and be difficult to diagnose, but it quickly gets much worse. The symptoms and signs may not all show up at once, and the illness may develop gradually over a few days, or much more quickly – over a few hours. People with meningococcal disease may have some or all of the following symptoms:
| Babies and children | Teenagers and adults |
|
Don’t wait – take action. If you or someone in your household is sick with one or more of the symptoms above, act immediately. Ring a doctor, medical or after-hours centre or the free Healthline number (0800 611 116) right away, day or night. If it's an emergency, call 111. |
Meningococcal disease bacteria live in the back of the nose and throat of about 1 in 10 healthy people, but only very rarely cause illness. The bacteria are spread by coughing, sneezing and intimate kissing. Very close or ongoing contact (eg, living in the same house) is usually required for the bacteria to spread to other people.
Meningococcal disease can affect anyone of any age, but those most at risk are:
- babies under 1 year of age
- Māori and Pacific Peoples children under 5 years of age
- teenagers and young adults
- people living in overcrowded households
- young people in hostels or residential centres
- people exposed to tobacco smoke
- people with a weakened immune system
- anyone with another type of respiratory infection, such as the flu (influenza).
People can catch meningococcal disease at any time of the year, but it’s more common in winter and spring.
Meningococcal disease can be difficult to diagnose because the signs and symptoms are often similar to those of other illnesses, eg, influenza (the flu). If your doctor suspects meningococcal disease, you will be referred to hospital where samples of your blood or cerebrospinal fluid (fluid around your spinal cord) will be collected and sent to the laboratory to check if an infection is present.
The infection is treated with antibiotics to kill the bacteria. It's important that treatment starts as soon as possible – meningococcal disease often develops quickly over a few hours and can cause serious disability or even death. If your doctor suspects you have meningococcal disease, they will give you antibiotics right away. Antibiotics help reduce the risk of complications and death.
Meningococcal disease bacteria can be spread from person to person by coughing, sneezing and kissing. Therefore, to prevent the spread, cover your nose or mouth when you sneeze or cough, and wash and dry your hands well.
What if I come into contact with someone who has meningococcal disease?
If you come into close contact with someone who has meningococcal disease, you're at the highest risk of developing the infection during the 7 days after the person developed symptoms. The local public health service follows up people who have recently come into close contact with anyone who has developed meningococcal disease and may provide you with preventive antibiotics. The antibiotics stop the spread of the disease, but you may still be at risk of getting the infection. This means you still need to watch for any symptoms, and get medical help quickly.
Vaccines are available to prevent against meningococcal disease. They protect against most, but not all types of meningococcal disease. In Aotearoa New Zealand vaccination is free for groups of people with a high risk of meningococcal disease. This includes:
- babies under 12 months of age as part of the National Immunisation Schedule(external link) (children under 5 years of age who haven't had all their doses can catch up for free until 31 August 2025)
- people from13 to 25 years of age who are going into, or are in, their first year of a close-living situation
- tamariki and adults with high risk medical conditions.
Read more about the meningococcal vaccine and who is eligible for it.
Meningococcal disease(external link) Health New Zealand | Te Whatu Ora, NZ
Meningococcal disease(external link) Immunisation Advisory Centre, NZ
Meningococcal disease(external link) KidsHealth NZ
Resources
Meningococcal disease [PDF, 1.8 MB] Health Promotion Agency and Health New Zealand | Te Whatu Ora, NZ, 2023
Meningococcal disease factsheet – don't wait, take action(external link) HealthEd, NZ, English, te reo Māori, Tongan, Samoan
Meningococcal disease – know the symptoms(external link) Health Promotion Agency, NZ English(external link), te reo Māori(external link), Samoan(external link), Tongan(external link)
References
- Meningococcal disease(external link) Immunisation Handbook, NZ
- Te mate meningococcal – meningococcal disease(external link) Health New Zealand | Te Whatu Ora, Health Information and Services, NZ
Messaging for healthcare professionals on meningococcal disease (August 2019)
- There has been a significant increase in Neisseria meningitidis serogroup W (MenW) in Aotearoa New Zealand since mid-2017.
- This particular strain of MenW affects all age groups and is associated with a high case-fatality rate.
- Health New Zealand | Te Whatu Ora is requesting that healthcare professionals remain alert to the symptoms of meningococcal disease as early intervention is essential.
Read more: Messaging for healthcare professionals on meningococcal disease(external link).
Clinical resources
Meningococcal invasive disease(external link) Te Mana Ora Community and Public Health, NZ
Meningococcal – information for health professionals(external link) Health New Zealand | Te Whatu Ora
Group B Meningococcal Disease in New Zealand(external link) Research review educational series
Brochures
New Zealand Government and Health New Zealand | Te Whatu Ora, NZ, 2023
Meningococcal disease factsheet – don't wait, take action
HealthEd, NZ, 2023
Meningococcal disease – know the symptoms
Health Promotion Agency, NZ, 2022 English, te reo Māori, Samoan, Tongan
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:







