Breast abscess
Key points about breast abscess
- A breast abscess is a painful, pus-filled lump that develops under the skin of your breast.
- Breast abscesses are common when you're breastfeeding, but can also occur at other times for males and females.
- They are mostly caused by an infection, where bacteria gets into your breast. This can be through a sore or cracked nipple or a nipple piercing.
- See your healthcare provider if your breast is red, swollen or sore.
- The main treatment for a breast abscess is to drain away the pus from the abscess.

A breast abscess is a painful, pus-filled lump that develops under the skin of your breast. They’re common if you’re breastfeeding, but can also occur in people with breasts who aren’t breastfeeding.
They’re often linked to mastitis, which is inflammation of your breast tissue, particularly the milk ducts and glands if you’re breastfeeding. Mastitis is due to inflammation, and doesn't always involve infection which needs antibiotics to resolve. Read more about mastitis.
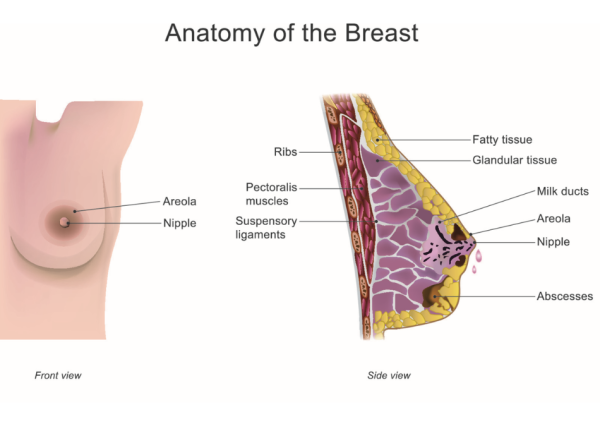
Image credit: Depositphotos
Most breast abscesses are caused by a bacterial infection.
If you have breast inflammation (mastitis) that becomes infected, this can sometimes go on to become an infected collection of fluid in your breast, which is an abscess.
Infections can occur when bacteria from your skin's surface or baby's mouth enter the milk ducts of your breast. If the infection isn’t treated, an abscess can form. Getting treatment for infected mastitis as soon as possible can help reduce your risk of getting an abscess. Sometimes an abscess can still form if treatment isn’t started quickly enough or if the antibiotics are not the right ones for the bacteria involved.
If you’re not breastfeeding you can get a breast abscess if bacteria enter your breast, such as through a sore or cracked nipple or a nipple piercing. Occasionally it can be because of an issue deeper in your breast.
Breast abscesses are hard, painful lumps in the breast that may also:
- be red or swollen
- feel hot
- have pus or discharge from the nipple
- be associated with a fever (high temperature), chills and a general feeling of being unwell.
Always see your healthcare provider if you notice any changes to your breasts, such as a breast lump or discharge (leaking fluid) from your nipples or if you have any redness that doesn’t go away with treatment. Occasionally, these symptoms could be a sign of breast cancer.
See your healthcare provider if your breast is red or swollen. They will examine your breasts and, if they think you have a breast abscess, they may arrange for aspiration of the lump to confirm if it is. An aspiration involves putting a needle in the swollen area to check if the lump is filled with pus. When you’re breastfeeding you can develop a cyst filled with milk (galactocele). This isn’t a breast abscess but it may still need treatment.
If the diagnosis isn't clear, your healthcare provider may also send you for an ultrasound scan of your breast to confirm whether or not the pain and swelling is caused by an abscess. Sometimes ultrasound is used to guide aspiration or drainage of an abscess as well.
If you have a breast abscess, you’ll usually be referred to the hospital surgical department for treatment.
The main treatment for a breast abscess is to drain away the pus from the abscess using needle aspiration. To do this, a local anaesthetic medicine is injected to numb the skin over your infected breast tissue, and the pus is drained using a needle and syringe.
You can take paracetamol or ibuprofen to relieve pain and fever. These medicines are considered safe if you're breastfeeding.
If you have multiple abscesses, or if the abscess is large or isn’t getting better with repeated aspiration treatments, surgical drainage (an operation) is needed. You’ll also be given antibiotics, often into your veins (IV).
If the abscess is large, it will need a bigger cut to let the pus drain out. After the infected area has been drained, it may be left open and packed with sterile gauze or closed with a small tube left in so the pus can drain out.
You may be prescribed a course of antibiotics after aspiration or surgical drainage. The full course of antibiotics needs to be taken as directed.
If you’re breastfeeding or lactating, you’ll still need to drain milk from your breast after aspiration or surgery (see below). Usually, you can continue breastfeeding after the surgical drainage when you’re taking antibiotics. Talk to your healthcare provider about continuing to breastfeed and ask for support with this if needed (see below).
If you have a breast abscess, you can usually continue breastfeeding unless you’re feeling very unwell, the abscess is very close to your nipple or you’ve had surgery to remove the abscess that makes feeding impossible.
If you’re breastfeeding, it's important to keep regularly feeding your baby or expressing milk as normal. Overfeeding or trying to empty your breast with a breast pump to try and get rid of the inflammation will actually make the symptoms worse. This is because blood flow and milk production will increase and put more pressure on your breast tissue. You may notice a drop in milk production at first, but this will return to appropriate levels once the inflammation has settled.
The following things can help if you’re breastfeeding with an abscess before and after treatment.
- Place ice or cold compresses/packs on the affected area, avoiding the nipple, for 20 minutes every hour, or more often if you want to. This helps to reduce blood flow and inflammation. It’s important not to apply heat as this can make things worse.
- Try lymphatic drainage techniques – gentle breast stroking helps reduce swelling. Using a light touch, with similar pressure to what you’d use to stroke a cat, stroke your breast from your nipple to your armpit and collarbone. You can do this as often as you like, and especially before breastfeeding or pumping. See the video below. Deeper massage or using vibrating or commercial massage devices can damage the breast tissue.
- Hand express a small amount of breast milk before breastfeeding if your breasts are too full with milk or if it hurts too much to feed. This will make your breasts less full and may make it easier for your baby to feed.
- Avoid pumping if possible as it can injure your breasts and nipples. Don’t pump large amounts of milk to store. If you have too much milk, get help from your midwife or a lactation consultant to reduce milk production (see support below).
- Try feeding from the healthy breast. Then, after your milk is flowing, breastfeed from the affected breast until it feels soft.
- Always wear a well-fitted, supportive bra.
Nicotine is associated with high rates of getting mastitis and breast abscess again so consider stopping smoking if you smoke.
See your healthcare provider immediately if any of your previous mastitis or abscess symptoms return, or if you develop any new symptoms.
Support
See the mastitis page for links to breastfeeding support services.
Video: Massage and lymphatic drainage for engorgement and mastitis
(Lucy Webber IBCLC, UK, 2023)
Apps reviewed by Healthify
You may find it useful to look at some breastfeeding apps.
Resources
Breastfeeding your baby(external link) HealthEd, NZ, 2021 English(external link), Chinese (simplified)(external link), Korean(external link), te reo Māori(external link), Samoan(external link), Tongan(external link)
Mastitis in breastfeeding(external link) Academy of Breastfeeding Medicine, US, 2023
Mastitis and sore breasts(external link) La Leche League International
Apps
References
- Mastitis and breast abscess(external link) Auckland Regional HealthPathways, NZ, 2024
- Mastitis and breast abscesses(external link) Health New Zealand | Te Whatu Ora
Clinical resources
Mastitis and breast abscess(external link) Health New Zealand | Te Whatu Ora, 2024
Mitchell KB, Johnson HM, Rodríguez JM, et al. Academy of Breastfeeding Medicine clinical protocol #36 – the mastitis spectrum, revised 2022(external link) Breastfeed Med. 2022;17(5):360–376S
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Angharad Dunn, GP, Wellington
Last reviewed:





