If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Mastitis | Ū kakā
Key points about mastitis
- Mastitis (ū kakā) is when your breast or part of it becomes inflamed (swollen, red, hot and painful). It usually gets better when the inflammation is treated and antibiotics are not needed in most cases.
- It's common in the first 4 weeks of breastfeeding as this is when breastfeeding/latching problems and breast engorgement often occur.
- Talk to your midwife or doctor if you get a sore breast, a tender red, lumpy area in your breast, have a fever or feel unwell with 'flu-like' symptoms.
- Don't stop breastfeeding. Continuing to breastfeed normally helps improve mastitis.
- Ease symptoms by applying ice, resting and taking pain relief.

Mastitis, or ū kakā, is when your breast or part of it becomes swollen, red, hot and painful.
It's common in the first 4 weeks of breastfeeding as this is when breastfeeding and latching problems often happen and your breasts can get engorged (very full of milk).
Mastitis usually gets better when the inflammation is treated. Antibiotics are not usually needed.
Talk to your midwife or healthcare provider if you get a sore breast, a tender red, lumpy area in your breast, have a fever (high temperature) or feel unwell with 'flu-like' symptoms.
While mastitis is common in the first month of breastfeeding, it can also occur at any stage when you are lactating (producing milk) and particularly when the number of breastfeeds or milk expressions is suddenly reduced. It can also happen if you are producing more milk than your baby needs, known as hyperlactation.
Symptoms of mastitis include:
- a sore breast
- a lumpy area that's usually red and tender
- fever (a high temperature)
- chills
- feeling unwell with 'flu-like' symptoms, such as tired, aching, run-down.
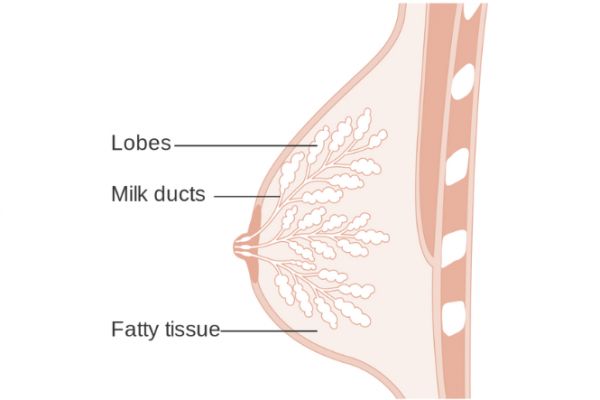 Image credit: CRUK, Wikimedia Commons
Image credit: CRUK, Wikimedia Commons
- Mastitis occurs when milk ducts in your breast become inflamed and the tissue around them becomes swollen. This causes the ducts to become narrower and the flow of milk towards the nipple slows down. Milk is still being produced but can't flow out as easily, so the affected part of the breast also becomes inflamed.
- Mastitis is inflammation of the breast tissue. It's not necessarily caused by an infection. Skipping feeding or pumping may cause redness and discomfort – this is inflammation, not infection.
- If inflammatory mastitis gets infected by bacteria you'll need to be treated with antibiotics. Sometimes bacterial mastitis can result in a breast abscess.
The following are the key ways of managing mastitis:
- Feed your baby as usual, don't over-feed or over-use a breast pump.
- Take paracetamol and ibuprofen (for pain relief and to reduce inflammation).
- Apply ice or another frozen item (eg, frozen peas) to the affected part of your breast – cold reduces pain and inflammation. Wrap the ice in a cloth before using and apply for about 10 minutes in every 30 minutes.
- Avoid heat to the breast.
- DO NOT use massage.
- Try lymphatic drainage – gentle breast stroking helps reduce swelling. Using a light touch, with similar pressure to what you would use to stroke a cat, stroke your breast from your nipple to your armpit and collarbone. You can do this as often as you like, and especially before breastfeeding or pumping. See the video below.
If you have a fever (temperature over 38.5°C) or your mastitis symptoms are not getting better in 24 hours it's important you talk to a healthcare provider. They may need to check and treat you for a bacterial infection or breast abscess. Read more about breast abscess.
Video: Massage and lymphatic drainage for engorgement and mastitis
- If you are having breastfeeding problems, ask your midwife for help. You might need a referral to a lactation consultant(external link) for more help.
- You can phone Plunketline(external link) on 0800 933 92 anytime day or night for advice about breastfeeding. You can also talk to your midwife, doctor or Plunket nurse.(external link)
- Some regions have Kaupapa Māori breastfeeding support. If you're interested in accessing Kaupapa Māori breastfeeding support, ask your midwife or local hauora service what's available in your region. Some of the services available are:
- Ūkaipō(external link) in Canterbury
- Te Tohu O Te Ora O Ngāti Awa(external link) in the Eastern Bay of Plenty
- Māori and Pacific Breastfeeding Service(external link) in Wellington
- B4Baby(external link) in South Auckland.
- Other groups to contact include La Leche League NZ(external link).
- You can also search the Women's Health Action(external link) site to find breastfeeding support.
- NZCLA provides a list of lactation consultants available in Aotearoa New Zealand(external link).
- A range of resources is listed on the Health New Zealand | Te Whatu Ora problems with breastfeeding(external link) page.
Apps reviewed by Healthify
You may find it useful to look at some Breastfeeding apps.
Find your breastfeeding support(external link) Women's Health Action, NZ
Breastfeeding – wide range of resources(external link) Health New Zealand | Te Whatu Ora
Breastfeeding – beginners guide [PDF, 889 KB] Auckland DHB and Waitematā DHB, NZ, 2021 (Also available in Chinese [PDF, 1.1 MB])
Mastitis in breastfeeding(external link) Academy of Breastfeeding Medicine, US
Apps
References
- Mitchell KB, Johnson HM, Rodriguez JM, et al. Academy of Breastfeeding Medicine Clinical Protocol #36: The mastitis spectrum, revised 2022(external link) Breastfeeding Medicine 2022;17(5):360-376
- Management of hyperlactation(external link) Guideline Central, US, 2020
- Mastitis and breast abcessess(external link) Health New Zealand | Te Whatu Ora, 2023
Key points of new protocol:
Mastitis:
- is a spectrum condition
- is not helped, and is likely to be worsened, by deep massage
- may elicit a systemic response that is not necessarily infective
- mostly resolves with conservative care
- is not the same as normal lactational glandular tissue which can feel ‘lumpy’ and tender
- does not develop into infection in a period of hours
- is not caused by retrograde spread of bacteria from a damaged nipple
- is not caused by mammary candidiasis
- is not helped by instructions to have baby ‘drain’ the breast, ‘dangle’ feeds or topical applications
- does not require investigations of c-reactive protein or white blood cell count, since these are markers of inflammation not specific for infection.
Summarised from: Mitchell KB, Johnson HM, Rodriguez JM, et al. Academy of Breastfeeding Medicine Clinical Protocol #36: The mastitis spectrum, revised 2022(external link) Breastfeeding Medicine 2022;17(5):360-376
Resources
Management of hyperlactation(external link) Guideline Central, US, 2020
Mastitis and associated complications(external link) Physician Guide to Breastfeeding, US
Apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Claire Salter, Pharmacist, Tauranga; Cara Hafner, Registered Nurse and Lactation Consultant, NZ Breastfeeding Alliance, Christchurch
Last reviewed:
Page last updated:





