Anaphylaxis is a preventable and treatable event. Knowing the trigger(s) is the first step in prevention. Everyone at risk needs to know how to avoid food allergens and/or other triggers.
However, because accidental exposure is possible, you and your child need to be able to recognise symptoms of anaphylaxis and be prepared to give adrenaline according to your anaphylaxis action plan.
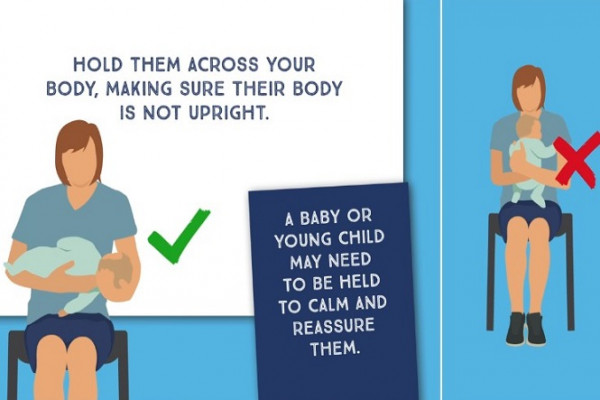
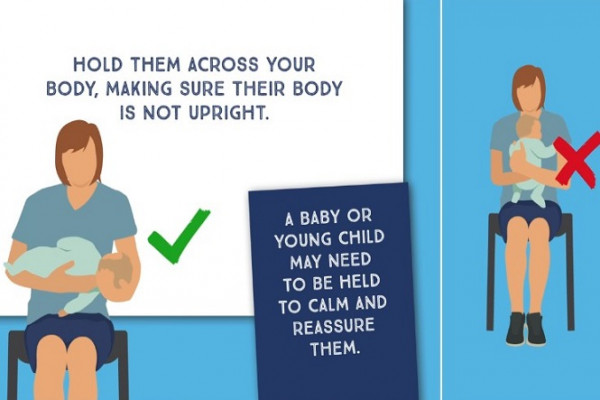
How to position a child or an adult having a severe allergic reaction (anaphylaxis)
Please click the image below and scroll down on the new page to play the animation.
 (external link)(external link)
(external link)(external link)
(Australasian Society of Clinical Immunology and Allergy)
If you have had anaphylaxis for the first time, after those immediate steps and then getting emergency medical care, as part of your treatment plan you need to:
- see a specialist to find out your triggers
- work out an anaphylaxis action plan(external link) with your healthcare provider
- attend follow-ups if required by your healthcare provider
- get educated on how to avoid triggers and use an adrenaline auto-injector if you are prescribed one
- ask your doctor or nurse specialist for an asthma management plan if you or your child also has asthma.
The Australasian Society of Clinical Immunology and Allergy (ASCIA) provides free online training on anaphylaxis for patients, families and the community.(external link)(external link)
Adrenaline is the first-line treatment for anaphylaxis
Adrenaline is the treatment for anaphylaxis. Adrenaline works by quickly reversing the effects of anaphylaxis.
Adrenaline can be easily given using an auto-injector such as an EpiPen (the only one available in Aotearoa New Zealand). The auto-injector injects a single, pre-measured dose of adrenaline into your muscle. If you're at risk of anaphylaxis, then your healthcare provider might ask you to carry an auto-injector with you. Deaths from anaphylaxis are more common away from home and when adrenaline is either not used or is delayed.
If you or your child are prescribed an adrenaline auto-injector, it is important to learn and practise how to use it. You can register your EpiPen with My EpiPen(external link) and receive a free trainer pen.
Don't use antihistamines
Don’t use antihistamines to treat anaphylaxis – giving adrenaline quickly is the only treatment for anaphylaxis. Anaphylaxis is a potentially life threatening, severe allergic reaction and should always be treated as a medical emergency.