Wisdom teeth
Also known as third molars
Key points about wisdom teeth
- Wisdom teeth are the teeth right at the back of your mouth. They're usually the last teeth to come through.
- There isn't always enough room in the mouth for them to grow properly, and this can cause a few different sorts of dental problems.
- On this page you can read about when and how wisdom teeth are removed, what to expect afterwards and how you can look after yourself.
Wisdom teeth are the molars right at the back of your mouth. They're usually the last teeth to come through and you usually get them when you're 17 to 25 years of age. However, not everyone has them or has problems with them.
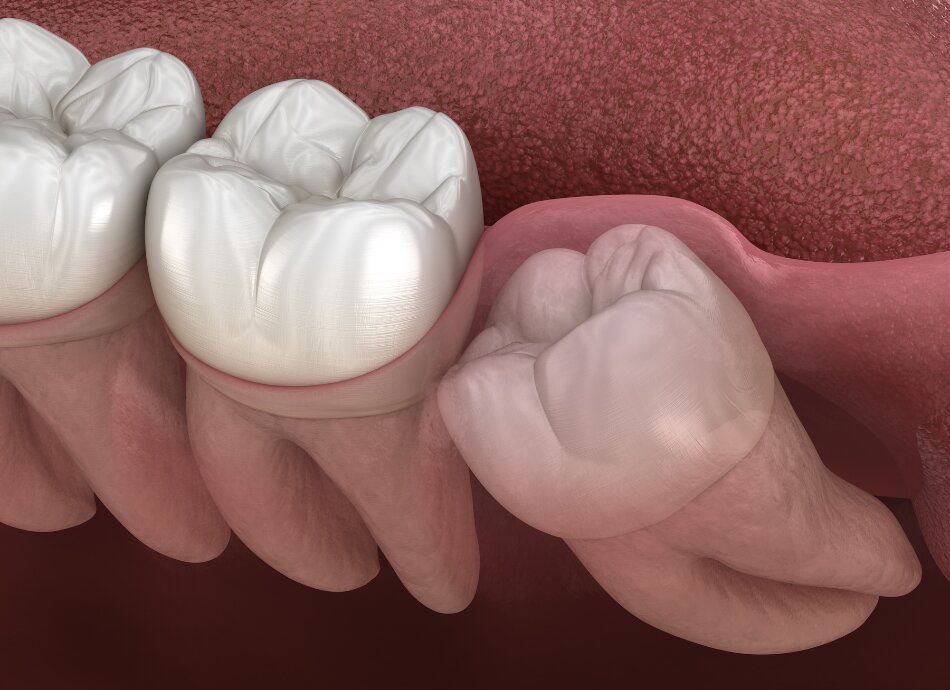
There isn't always enough room in the mouth for them to grow into place properly, and this can cause dental problems with the gum around them and with the teeth beside them.
If you have no pain or any other problems with your wisdom teeth, continue with your usual oral health care and dental visits.
If you have pain or infection, make an appointment to see your dentist as soon as possible. They may take an X-ray of your mouth to give a clearer view of the position of your teeth.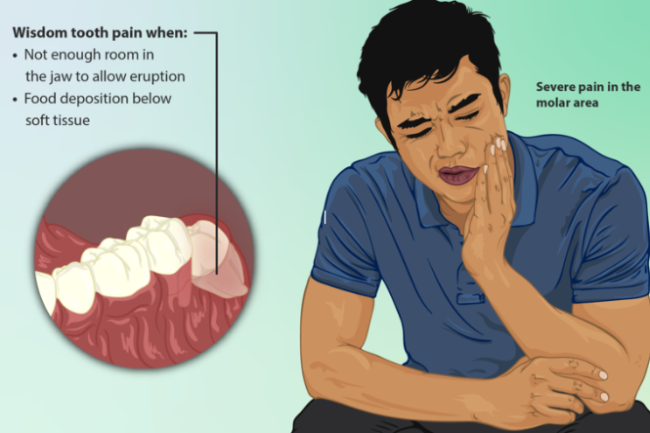
Image credit: Wikimedia Commons
If they're not causing you any problems, there is often no need to get your wisdom teeth removed. However, you may not notice some problems, eg, decay, so it’s important to see your dentist regularly. Upper and lower wisdom teeth are different, so sometimes lower wisdom teeth need to be removed but not the upper ones, or the other way around.
If it’s likely that your wisdom teeth will cause problems in the future, your dentist may recommend you have them removed before you experience problems. It's also easier to remove wisdom teeth when you are younger as bone is less flexible and healing is slower in older people.
If your wisdom teeth are to be left in place, but are at risk, you will need to get your teeth checked regularly.
Video: Wisdom teeth
(NHS Choices, UK, 2015)
Your wisdom teeth usually don't need to be removed unless they're impacted (can't come through properly) and causing problems. Some problems associated with wisdom teeth can be managed with antibiotics, antiseptic mouthwash, and by keeping the area very clean.
Your dentist may recommend having your wisdom teeth removed if you develop:
- tooth decay
- abscesses (pus in your wisdom teeth or the surrounding tissue)
- an infection of your gum caused by an erupting wisdom tooth (pericoronitis)
- periodontal (gum) disease, such as pericoronitis, or an infection of your connective tissue (cellulitis)
- an infection of your bones (osteomyelitis)
- cysts or tumours involving the tooth
- teeth that obstruct other surgery
- or, if you plan to travel in less-developed countries for an extended period of time where treatment might be hard to get if your teeth or gums become a problem.
Wisdom tooth removal may be a simple or a complicated procedure, depending on the position of your teeth:
- Routine, uncomplicated removal of a single wisdom tooth can usually be done in your dentist’s surgery, using a local anaesthetic.
- Less routine removal may require the use of a sedative combined with a local anaesthetic. Some dentists are qualified to use sedation in their surgery.
- Complicated surgery, or the removal of a number of wisdom teeth, may require IV (intravenous) sedation or a general anaesthetic. This must be done by an appropriately qualified oral surgeon with an anaesthetist and theatre staff.
Having an anaesthetic is usually safe and major problems are rare. However, there are some risks associated with having a general anaesthetic for very young children, older adults and people with other health problems. Find out more about anaesthesia.
Afterwards
As with any surgical procedure, you're likely to have some swelling, bleeding, bruising and discomfort after having your wisdom tooth removed. You may also have some temporary numbness of your tongue, lip or chin, which in rare cases can be permanent.
When removing an impacted wisdom tooth, it may be necessary to make a cut in your gum, remove bone and cut the tooth into pieces in order to remove it. You may be left with sutures (stitches) after the extraction.
As removal carries some risk of complications, your dentist will weigh up the risks and benefits and advise you of the best course of action.
Specific risks of having wisdom teeth removed include:
- Infection of the soft tissue or underlying bone. Signs include a high temperature, yellow or white discharge from the extraction site, and persistent pain and swelling. It's normal for the area to look grey or white, but not to have discharge draining from it.
- Haemorrhage (bleeding) – more than just an ooze of blood.
- Dry socket: This is a painful condition that occurs more often with tooth extractions in the lower jaw and in people who smoke. With dry socket, no blood clot forms (or it's washed away by rinsing too early) and the normal healing process is prevented
- Trismus (lockjaw): This is a painful condition where the chewing muscles of your jaw become contracted and sometimes inflamed, preventing your mouth from fully opening.
- Nerve damage: Great care is taken to avoid the nerve being injured, using X-rays and 3D scanning to see if the nerve is near the root tips. However, sometimes damage or bruising can happen causing tingling or numbness to your tongue, lip or chin. Rarely, this can be long-term or permanent.
See your dentist if you have signs of infection after having your wisdom teeth removed, or if you're bleeding heavily from the extraction site.
The risks associated with wisdom teeth extraction are increased through stress, poor oral hygiene and getting an upper respiratory tract infection. There are things you can do to reduce these risks:
- Take time off work or study to recover.
- Rest for the first 24 hours – overexerting yourself can put pressure on the surgery site and increase pain and bleeding.
- Keep the area around the extraction clean – follow your dentist’s advice.
- Avoid chewing on the surgery site for 24 hours – try switching to a soft diet for a few days.
- Avoid smoking, which increases your risk of bleeding and slows healing.
- Avoid alcohol as this can lead to postoperative bleeding.
- Avoid sucking or spitting as this can promote bleeding and dislodge the blood clot, which may lead to dry socket.
- Control swelling by using an ice pack.
- Manage any pain with an anti-inflammatory medication, eg, ibuprofen (not aspirin, which can increase bleeding).
- After 24 hours, start regular, gentle rinses of your mouth with a warm saline (salt water) solution, if recommended by your dentist.
- Contact your doctor or dentist if you develop any unusual bleeding, swelling or pain.
To prevent tooth decay, pain and infection, take extra care of wisdom teeth that haven't fully come through.
- Floss between all your teeth, especially between the wisdom teeth and the teeth in front of them.
- Make sure that your toothbrush reaches all the way to the back when brushing your teeth.
- Rinse with a saline solution (salt dissolved in warm water) if you have any early signs of infection, eg, redness, heat or tenderness in the area.
- Get good advice from your dentist about how exactly to care for the situation in your mouth. We're not all the same and home care can be different for different people.
People on low incomes who have a Community Services Card may be able to get free emergency dental care, eg, pain relief or extractions. These services may be provided by public hospitals or dentists contracted by your health district. You can find out who provides this service by phoning 0800 TALK TEETH/0800 825 583.
You may still need to pay some of the treatment cost, and you may only get support for an infection but not for extraction. Find out more from Work and Income on their dental treatment(external link) page.
The following links provide further information about wisdom teeth. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Wisdom tooth removal(external link) Mayo Clinic, US
Impacted wisdom teeth – do I need them removed?(external link) Mayo Clinic, US
Wisdom teeth(external link) Patient Info, UK
Your oral health – teens(external link) Healthy Smiles, NZ
References
- Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth.(external link) Mettes TDIRKG, Ghaeminia H, Nienhuijs MEL, Perry J, van der Sanden WJM, Plasschaert A. Cochrane Database of Systematic Reviews 2012, 6, Art. No. CD003879.
- Wisdom teeth removal(external link) NHS, UK, 2021
- Publicly funded dental care(external link) Health New Zealand | Te Whatu Ora, 2024
- Wisdom tooth removal – complications(external link) NHS, UK, 2021
Oral health(external link) BPAC, NZ, 2009
Dental and oral health overview(external link) National Institute Clinical Evidence, UK, 2014
Guidance on the Extraction of Wisdom Teeth(external link) NICE, UK 2000
Colquhoun A. The third molar dilemma – Leave? Or extract? NZDA News. 2017 May;183:27-30. The full article is available to members of the NZ Dental Association(external link)
Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth(external link) Cochrane Oral Health Group, 2016
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Sophie McKenna, General Dental Surgeon
Last reviewed:





