A ventilator is a machine that assists or takes over the work of breathing when you can't breathe enough on your own, to make sure your body gets enough oxygen and that carbon dioxide is removed.
There are 2 types of mechanical ventilation using ventilators:
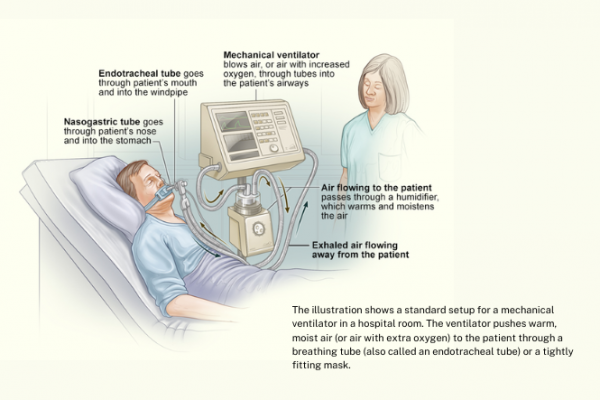
- non-invasive ventilation uses a face or nasal mask
- invasive ventilation uses a hollow plastic tube inserted into your wind pipe (trachea).
Ventilators are used during surgery, when you're under anaesthesia and if a disease or condition impairs your lung function and makes it difficult or impossible for you to breathe normally. This may be the case if:
- you have a severe infection, such as with pneumonia or COVID-19
- you have an injury to your brain
- you're unconscious and unable to breathe on your own.
Being on a ventilator doesn't heal you, instead it gives your organs a chance to improve while medicines and treatments help you to recover.