Uveitis is a condition where there is inflammation inside your eye in the middle layer of tissue called the uvea.
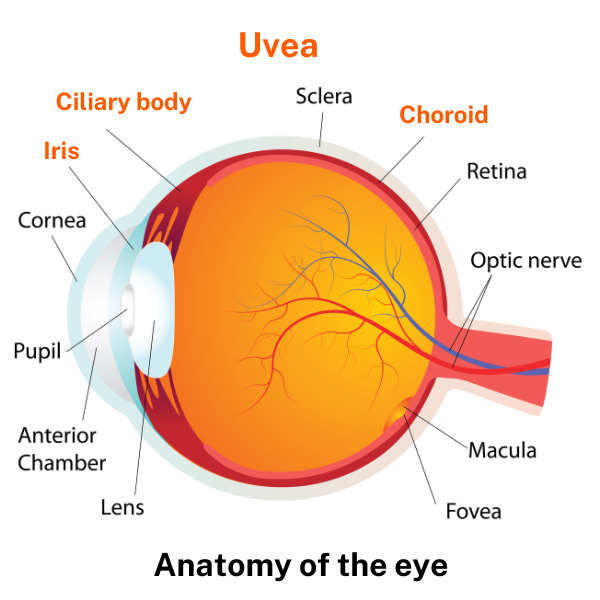
The uvea is the layer of the eye between the sclera (the outside white part of your eye) and the retina (the tissue inside at the back of your eye).
The most common type of uveitis is anterior uveitis which affects the iris at the front of your eye (also known as iritis). Uveitis usually affects 1 eye, but it can affect both. It’s most common in people 20 to 60 years of age but can happen at any age.
Symptoms of uveitis can start suddenly and include blurry vision, redness of your eye, eye pain, sensitivity to light and floaters (dark spots or squiggly lines that float across your vision). You can lose some of your vision if uveitis isn’t treated, so see your healthcare provider straight away if you have any of these symptoms.