If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Lenalidomide
Sounds like 'LEN-a-LID-oh-mide'
Key points about lenalidomide
- Lenalidomide is used to treat different types of cancer.
- Lenalidomide is also called Revlimid. From 1 August 2024 the funded brand of lenalidomide will be Lenalidomide Viatris.
- Find out how to take lenalidomide safely and possible side effects.

Lenalidomide is a medicine used to treat some types of cancers. It kills or stops the growth of cancer cells and blocks the development of new blood vessels which cancer cells need to grow and spread. Lenalidomide also works with your body's immune system to attack cancer cells.
In Aotearoa New Zealand, lenalidomide is funded for treating multiple myeloma and myelodysplastic syndrome for people who meet the eligibility criteria.
August 2024: The funded brand of lenalidomide is changingFrom August 2024, the funded brand of lenalidomide will be changing from Revlimid to Lenalidomide Viatris. This means your capsules will look different but will work the same way. There is the same amount of active ingredient (medicine) in each capsule. Lenalidomide Viatris is only available in Aotearoa New Zealand under a special programme.
Read more about the lenalidomide brand change(external link). |
The image below shows what the different strength of Lenalidomide Viatris capsules look like.
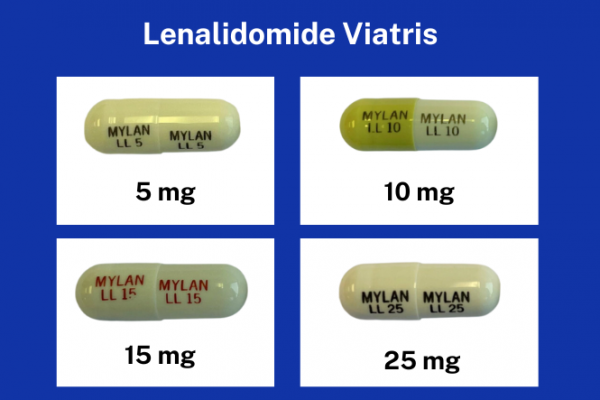
Image credit: Viatris and Healthify He Puna Waiora
- Always take your lenalidomide exactly as your doctor has told you. The pharmacy label on your medicine will tell you how much to take, how often to take it, and any special instructions.
- In Aotearoa New Zealand, lenalidomide is available as capsules in different strengths (5 mg, 10 mg, 15 mg and 25 mg).
- The dose of lenalidomide is different for different people, depending on what it's being used for and your response to treatment.
- Your prescriber may adjust your dose depending on the result of blood tests and any side effects you may have.
- Take care when handling the capsules: Remove your capsules carefully from the packaging and wash your hands afterwards.
- Timing: Take lenalidomide once a day, at the same time each day.
- Swallow the capsules whole, preferably with water: Don't open, break or chew the capsules. If powder from a broken lenalidomide capsule touches your skin, wash the skin immediately and thoroughly with soap and water.
- Food: Take your dose on an empty stomach, either 1 hour before or 2 hours after eating food.
- Missed dose: If you forget to take your dose, take it as soon as you remember. But if it's less than 12 hours until your next dose, just take the next dose at the right time. Don't take double the dose.
Pregnancy Prevention Program
Lenalidomide is only available in Aotearoa New Zealand under a special programme.
- Women and men must be enrolled and agree to the conditions of the program before they can get lenalidomide.
- Only prescribers registered with the pregnancy prevention program can prescribe this medicine.
- Only pharmacies/pharmacists registered with pregnancy prevention program can dispense this medicine.
Females
It's very important to make sure you don't become pregnant.
Note: Even if you're not having regular periods or are near menopause, you may still be able to become pregnant.
- You must use effective contraception at least 1 month before, during, and for at least 1 month after treatment, including during lenalidomide dose interruptions.
- You must have a pregnancy test before starting treatment to check that you're not pregnant and be re-tested every month (before each dispensing) and 1 month after the end of treatment.
- Note: The pregnancy test must be organised by your doctor. You can't use the home pregnancy test kits available from a pharmacy or supermarket. This is to make sure that the test is done accurately and your doctor can give you immediate advice based on the results.
- You should start your lenalidomide treatment as soon as you have had a negative pregnancy test result.
- Make sure you get your lenalidomide within 7 days of it being prescribed, or you will need a new pregnancy test to get a new prescription.
Contraception: Not all types of contraception are suitable during lenalidomide treatment. Only the options with a very low failure rate (less than 1%) are recommended. This means that with perfect use, fewer than 1 out of 100 women using the method will become pregnant in a year.
Recommended contraception:
- Hormone releasing intra-uterine device (IUD) eg, Jaydess and Mirena.
- Hormone implant (Jadelle).
- Depot hormone injection (Depot-Provera).
- Tubal ligation.
- Partner’s vasectomy (confirmed by 2 negative semen analyses).
- Progestogen-only oral contraceptive pill desogestrel (Cerazette).
Contraception that's not recommended:
- Copper IUD (increased risk of infections and bleeding).
- Combined oral contraceptive pill (because of increased risk of blood clots).
- Condoms (unreliable).
- Fertility awareness (unreliable).
You and your partner should talk to your doctor about suitable forms of contraception that you both find acceptable.
Males
Lenalidomide passes into human semen, so there is a risk that the medicine can be passed to partners who could become pregnant during sex. Therefore, it's important for men who are taking lenalidomide to use effective contraception to prevent pregnancy in their partners.
- If your partner is pregnant or able to become pregnant and doesn’t use effective contraception, you must use condoms during your treatment and dose interruptions and 7 days after you stop lenalidomide.
- Note: Even if you've had a vasectomy, you must use a condom throughout your lenalidomide treatment.
- If your partner does become pregnant while you're taking lenalidomide or within the 7 days after you have stopped taking lenalidomide, let your prescriber know immediately and your partner should also contact their doctor immediately.
- Don't donate blood or semen or sperm during treatment or treatment interruption, or for at least 1 week after stopping treatment.
- You must get your lenalidomide within 28 days of it being prescribed, or you will need a new prescription.
Handling and storing lenalidomide
- Store lenalidomide in the original, labelled container in a safe place, out of reach of children and pets.
- This medicine shouldn't be stored in a pillbox.
- Pregnant or breastfeeding women shouldn't handle the medicine for you.
- Healthcare providers, caregivers and family members should wear disposable gloves when handling the blister or capsule. Gloves should then be removed carefully to prevent contact with the skin, placed in a sealable plastic polyethylene bag and disposed of as advised by your healthcare team.
- Don't share your medicines with anyone else, even if they have similar symptoms to you.
- Ask your healthcare team where to return any unused medicine for disposal. Don't flush it down the toilet or throw it in the rubbish.
Vaccinations
- Since lenalidomide affects your immune system, you're at increased risk of infection. It's important that you're up to date with the annual flu vaccination and the COVID-19 vaccinations. These are non-live vaccines and they're safe to have while you're taking lenalidomide.
- You shouldn't be given any live vaccines, such as MMR (measles, mumps and rubella) and varicella (chickenpox vaccine), while you're receiving pomalidomide and for 6 months after treatment has stopped. Ask your healthcare team if you have questions.
Treatment delays
There may be times when your treatment is delayed. This can happen:
- if you get severe side effects
- if your blood counts are affected
- if you're finding it hard to cope with the treatment.
Your doctor will tell you if you need any delays to your treatment and the reason why.
Other medicines
Lenalidomide interacts with some medicines, herbal supplements and rongoā Māori, so check with your doctor or pharmacist before starting lenalidomide and before starting any new products.
Like all medicines, lenalidomide can cause side effects, although not everyone gets them. Because lenalidomide affects your immune system, it may cause a variety of side effects. It may also make you more unwell with other illnesses.
- You may experience side effects at any time during your treatment. Some side effects go away within a few days or weeks and some may be longer lasting.
- To monitor your side effects, you will need regular reviews and blood tests to check your liver, kidneys and blood before you start treatment and regularly while you are receiving treatment.
| Common side effects |
|
Report any side effects to your healthcare provider straight away even if they appear mild. Don't try to manage these side effects on your own:
|
Rare serious side effectsFor some people, these side effects could be life threatening. If you have any of the side effects mentioned below OR any new or worsening symptoms, contact your healthcare team or Healthline on 0800 611 116 straight away:
Note: This is not a full list of side effects and side effects can vary in different people. If you don't know whether your symptoms are side effects of the medicine, contact your healthcare team straight away. |
Revlimid(external link) Medsafe Consumer Information Sheet
Lenalidomide Viatris(external link) Medsafe Consumer Information Sheet
Contraception your choice – comparing typical effectiveness of contraceptive methods(external link) Sexual Wellbeing Aotearoa, NZ,
References
- Lenalidomide(external link) New Zealand Formulary
Brochures
Contraception your choice – comparing typical effectiveness of contraceptive methods
Sexual Wellbeing Aotearoa, NZ, 2021
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist; Joanna Buchanan, Oncology Pharmacist
Last reviewed:





