Rubella (German measles) is a rare virus nowadays, and most people have been vaccinated against it in childhood. Unlike the other tests, screening in pregnancy is done to check if you are immune to this virus, rather than checking if you are infected. Unfortunately, immunity from rubella vaccinations tends to decrease with time, so it is recommended that you are tested at the start of every pregnancy. If you do become infected with rubella while you are pregnant, it is usually mild for you. However, it can cause severe birth defects in your baby (eg, blindness, deafness or heart defects). If you are found to have no or low immunity to rubella, you will be recommended to have the vaccination. This vaccination is not given during pregnancy (as it is a live vaccine), but will be given soon after you have given birth, to protect any future pregnancies.
We're aware of a problem when trying to use Zero Data to link to Healthify. Zero Data is managed by Health NZ and we are working with them to get this fixed.
Pregnancy blood tests – screening for infections
Key points about screening for infections during pregnancy
- Pregnancy (antenatal) blood tests are carried out during pregnancy to check on the health of you and your pēpi.
- During your pregnancy, you will have blood tests to look for 4 infections that may affect your pregnancy or your unborn baby.
- These blood tests need to be done as early as possible in pregnancy.
- This is so treatment can be started early, if you need it, to reduce the risk of passing the infection on to your baby.

Syphilis is a sexually transmitted bacterial infection that used to be rare, but is becoming more common around the world. It causes long-term (chronic) infection if untreated, and many people are unaware that they have it, as initial symptoms of infection are mild. Chronic infection can cause severe damage to organs and death. If you become pregnant while chronically infected, it can pass through the placenta and infect your baby. It can cause a stillbirth or serious problems such or deafness, seizures or birth defects. If you are diagnosed with syphilis in pregnancy, you will be referred to a specialist to discuss treatment. This is with a course of antibiotic injections and, if given early enough, should prevent problems for you and your baby. You will also be recommended to have any sexual partners or previous children tested, so that they can be offered treatment as well.
Hepatitis B is a viral infection that can be acquired sexually or through contact with blood or body fluids from an infected person. It can also be passed from a mother to baby during pregnancy, and in many countries this is the most common way that people have been infected. You may or may not already be aware that you have been infected. Many people who have been infected do not get rid of it and become chronic ‘carriers’ of the infection, able to infect others. This can cause health problems for them (liver damage, liver cancer, early death). If you are a carrier and become pregnant, it can pass through your placenta to your baby. Most (up to 9 out of 10) babies born to mothers will be infected if no treatment is given, and if infected most (again up to 9 out of 10) babies will have chronic infection for the rest of their lives, with worse health effects than people who become infected as adults.
If you are diagnosed with Hepatitis B, all close household contacts should be tested for the virus, so that they can be offered treatment. In addition you will be asked to have another blood test to see what the level of virus in your bloodstream is. If it is high, you will be referred to a specialist to discuss treatment, which will both improve your long-term health and reduce the chance of infection for your baby. It is recommended that all babies in Aotearoa New Zealand are vaccinated against Hepatitis B with several doses of the vaccine starting at 6 weeks of age. If you are known to be a carrier, it is recommended that the vaccine is given to your baby shortly after being born, and an additional injection called immunoglobulin is given to increase the protection. These treatments greatly reduce the risk of your baby being infected, but a few babies are still infected despite them. Your baby should therefore be followed up and tested for infection after a few months so that any further monitoring or treatment can be started if required.

Image credit: Canva
Human Immunodeficiency Virus (HIV) is a virus that can be acquired sexually or through contact with infected blood or body fluids. It can cause a chronic infection which progresses to severe AIDS (Acquired Immunodeficiency Syndrome) and death if not treated. You may or may not know that you have already been infected.
If you are infected and become pregnant, it can infect your baby, either through the placenta, or more commonly during delivery or from breastfeeding. Around 1 in 3 or 4 babies born to mothers with HIV become infected if no treatment is given. With treatment of mother and baby, during pregnancy and after delivery, this risk reduces to about 1 in a 100 babies being infected.
If you are found to have HIV, you will be referred to a specialist to discuss treatment to reduce the health problems for you and your baby. You may be offered treatment for HIV for yourself while still pregnant (‘anti-retroviral’ tablets), which will be safe to take for the baby and reduce health problems for yourself. If the level of the virus is high in your blood stream you may be recommended to have a Caesarean section to deliver the baby, although some woman on treatment can deliver normally. You will be recommended not to breastfeed your baby, and your baby will receive anti-retroviral medicine and long-term follow up and testing. It is recommended that any sexual partners and former children are also tested, so that they can be offered treatment.
Pregnancy and newborn screening(external link) National Screening Unit, NZ
Rubella(external link) Immunisation Advisory centre, NZ
STDs during pregnancy(external link) Center for Disease Control and Prevention, US
Apps
Resources
Protect your unborn child – rubella(external link) HealthEd, NZ, 2020
Hepatitis B – Information for pregnant women(external link) HealthEd, NZ, 2023
Brochures
HealthEd, NZ, 2020
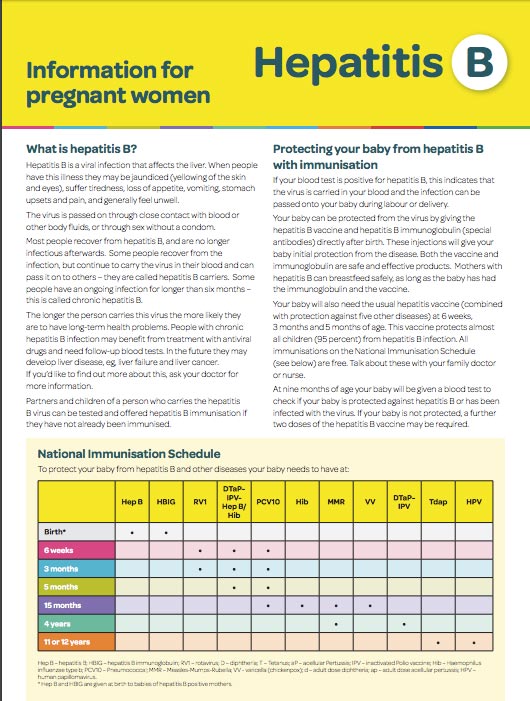
HealthEd, NZ, 2023
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Janet Crofts, Obstetrician, Auckland
Last reviewed:
Page last updated:





