You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Pancreatic cancer
Key points about pancreatic cancer
- Pancreatic cancer is a type of cancer that begins in your pancreas, an organ in your abdomen (tummy).
- Several types of tumour can occur in your pancreas, and they can be cancerous (malignant) or non-cancerous (benign).
- The most common type starts in the cells lining the ducts of your pancreas, it's mostly found in people over the age of 45 years.
- It doesn't generally cause symptoms in the early stages, later on a range of symptoms can occur including abdominal pain, appetite loss, unintended weight loss, yellowing of skin and eyes (jaundice), diabetes and fatigue.
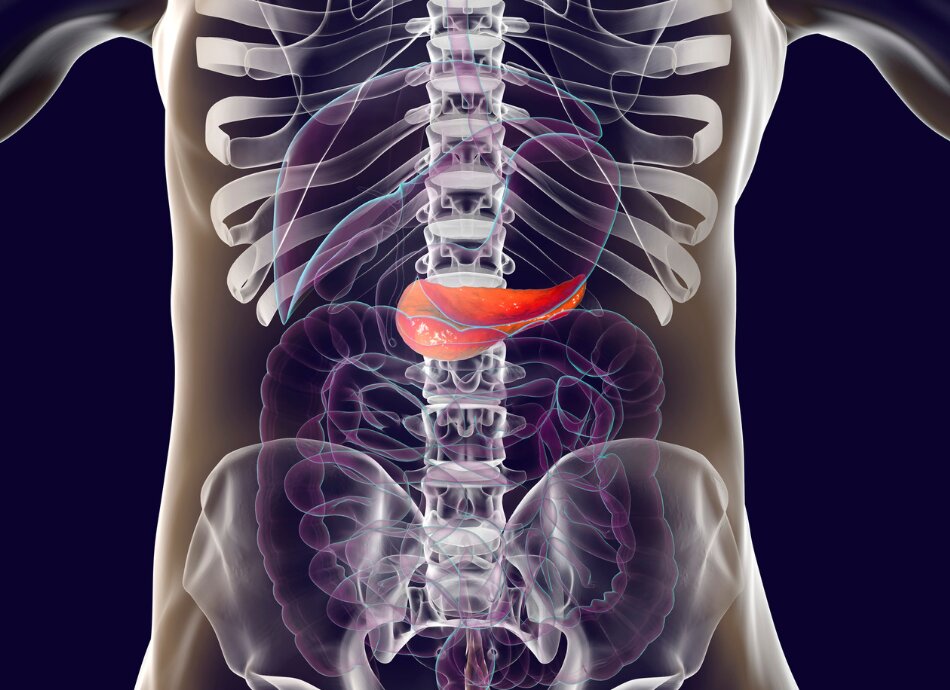
The pancreas is an organ that lies behind your stomach. It makes enzymes that help break down food so it can be digested. It also releases hormones, particularly insulin which is important for regulating the amount of glucose (sugar) in your bloodstream.
Several tumours can occur in your pancreas. These can be either cancerous or non-cancerous. The most common cancer starts in the cells that line the ducts of your pancreas. They carry digestive enzymes out of your pancreas into your duodenum (the first part of your small intestine). This is called pancreatic ductal adenocarcinoma.
Anyone can be affected by this cancer, but it is commonly found in people over the age of 45 years. Pancreatic cancer is slightly more common in Māori and Pacific Peoples.
Anything that can increase your risk is called a risk factor. Having one or more of these risk factors does not mean that you will develop pancreatic cancer. Even if you have no risk factors you can still develop pancreatic cancer.
Risk factors for pancreatic cancer include:
- smoking
- heavy drinking
- having a family cancer syndrome also linked to breast, bowel, prostate and ovarian cancer (BRACA 2 mutation or Lynch syndrome)
- diabetes
- chronic inflammation of your pancreas (pancreatitis)
- family history of pancreatic cancer
- obesity.
Pancreatic cancer does not cause many signs or symptoms in its early stages when it is most curable. This is because it does not generally cause symptoms until it has spread or the tumour is large enough to block the bile duct and cause jaundice (yellowing of your skin and the whites of your eyes).
The symptoms that occur with pancreatic cancer can also occur with lots of other conditions. They may include:
- abdominal pain, commonly radiating to your back
- loss of appetite
- unintended weight loss
- yellowing of your skin and the whites of your eyes (jaundice)
- light-coloured stools
- dark-coloured urine
- itchy skin
- new diagnosis of diabetes or existing diabetes that's becoming more difficult to control
- blood clots
- fatigue.
There is no examination specifically for the diagnosis of pancreatic cancer. Most people need to have several tests and scans to confirm a diagnosis of pancreatic cancer. These include:
- Blood tests including measuring CA19-9. CA19-9 is a protein that can be elevated in pancreatic cancer, but also in other non-cancerous conditions, eg, cirrhosis of your liver.
- Ultrasound is usually the first imaging investigation requested. If this is abnormal then a CT scan is usually requested. Depending on what this reveals an MRI or PET scan may be requested.
- In order to confirm the diagnosis, a sample of the tumour may be removed. This is done via endoscopic ultrasound and biopsy. An endoscope is a flexible tube that is passed through your mouth and down to your stomach. It has an ultrasound attached in order to obtain pictures of your pancreas and this can also be used to get a tissue sample.
If you are suspected to have pancreatic cancer, you will be referred to a specialist called a hepatobiliary surgeon. A team of health professionals with expertise and experience with pancreatic cancer will look after your care.
The treatment for pancreatic cancer depends on stage (how far it has spread), the severity of your symptoms and your preferences.
If you are jaundiced you may have treatment via another endoscopy to pass a small stent to relieve the blockage causing the jaundice.
Many surgeons perform a laparoscopy (keyhole surgery) to confirm that the cancer has not spread. If it hasn’t then surgery can be undertaken to remove the tumour.
Other treatment may include chemotherapy (medicines to destroy cancer cells) which can be given before or after surgery. There are many different types of chemotherapeutic drugs and what is recommended for you may be a single drug or a combination.
Some people may have radiotherapy (radiation treatment) recommended. This can also be before or after surgery. Occasionally it is given if people are not suitable for surgery to help minimise symptoms.
Unfortunately, pancreatic cancer has poor long-term survival as it is usually diagnosed when it has spread. If caught early it is curable. Prompt investigation of symptoms is important to ensure pancreatic cancer is diagnosed and treated as early as possible.
Australian NZ Gastro-Oesophageal Surgery Association(external link)
Pancreatic cancer(external link) Cancer Society, NZ
Resources
Living with pancreatic cancer: Information for patients and carers(external link) Avner Pancreatic Cancer Foundation, Australia
Living well with cancer – eating well [PDF, 5.5 MB] Cancer Society, NZ, 2020 Available in the following languages: English/Maori [PDF, 5.5 MB]
Living well with cancer – keeping active [PDF, 2.4 MB] Cancer Society, NZ, 2020 Available in the following languages: English/Te reo Māori [PDF, 2.4 MB]
Living well with advanced cancer(external link) Cancer Society, NZ, 2020
Side effects of cancer treatment – eating and mouth problems(external link) Cancer Society, NZ, 2020 Available in the following languages: English(external link) Māori(external link)
Coping with fever and nausea(external link) Cancer Society, NZ, 2019
Managing cancer pain(external link) Cancer Society, NZ, 2020
Talking to a friend with cancer(external link) Cancer Society, NZ, 2017
Brochures
Avner Pancreatic Cancer Foundation, Australia
Cancer Society, NZ, 2020
Cancer Society, NZ, 2020
Credits: Used with permission from Te Aho o Te Kahu | The Cancer Control Agency
Reviewed by: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Last reviewed:
Page last updated:





